10% longer.
Reduced food intake, known as dietary restriction, leads to a longer lifespan in many animals and can improve health in humans. However, the molecular mechanisms underlying the positive effects of dietary restriction are still unclear. Researchers from the Max Planck Institute for Biology of Aging have now found one possible explanation in fruit flies: they identified a protein named Sestrin that mediates the beneficial effects of dietary restriction. By increasing the amount of Sestrin in flies, researchers were able to extend their lifespan and at the same time these flies were protected against the lifespan-shortening effects of a protein-rich diet. The researchers could further show that Sestrin plays a key role in stem cells in the fly gut thereby improving the health of the fly.
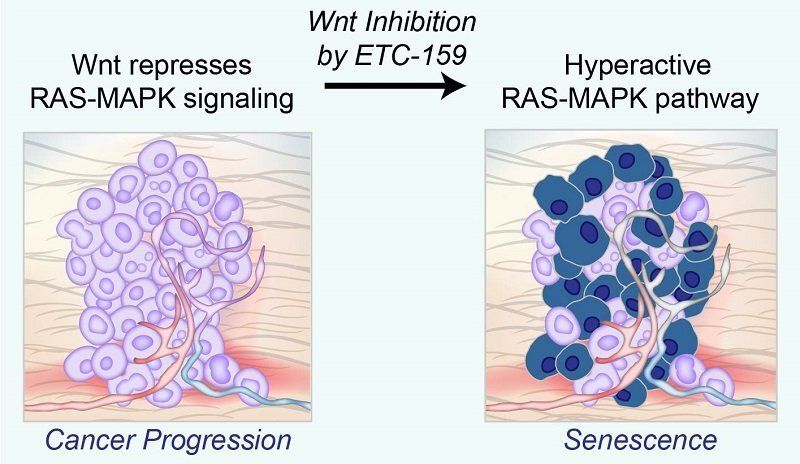
The health benefits of dietary restriction have long been known. Recently, it has become clear that restriction of certain food components, especially proteins and their individual building blocks, the amino acids, is more important for the organism’s response to dietary restriction than general calorie reduction. On the molecular level, one particular well-known signaling pathway, named TOR pathway, is important for longevity.
“We wanted to know which factor is responsible for measuring nutrients in the cell, especially amino acids, and how this factor affects the TOR pathway,” explains Jiongming Lu, researcher in the department of Linda Partridge at the Max Planck Institute for Biology of Aging. “We focused on a protein called Sestrin, which was suggested to sense amino acids. However, no one has ever demonstrated amino acid sensing function of Sestrin in a living being.” Therefore, Lu and his colleagues focused on the role of Sestrin in the model organism Drosophila melanogaster, commonly known as fruit fly.