Nad plus works for alzheimers.
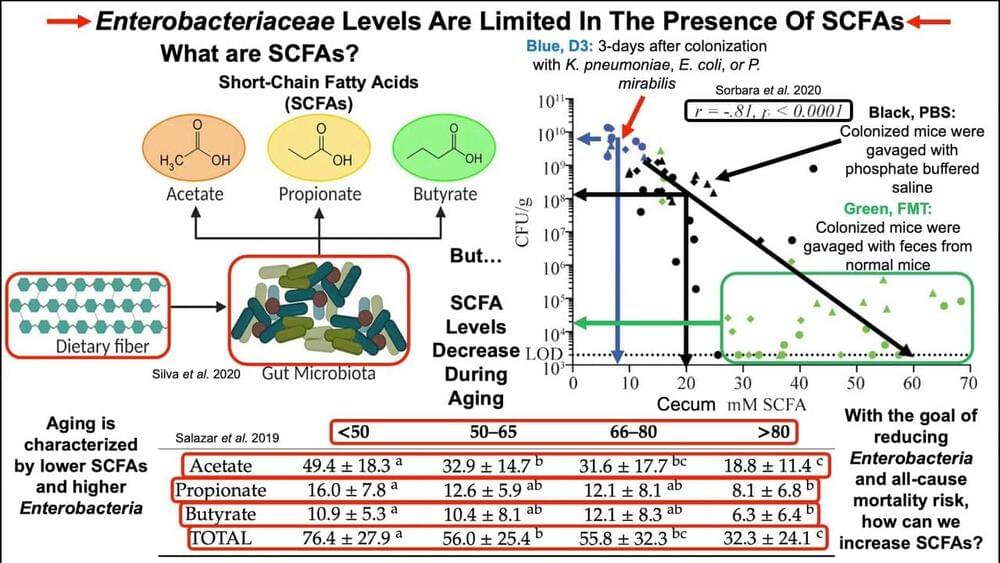
In June of 2,018 the World Health Organization (WHO) released the 11th edition of its International Classification of Diseases, and for the first time added aging.1 The classification of aging as a disease paves the way for new research into novel therapeutics to delay or reverse age-related illnesses such as cancer, cardiovascular and metabolic disease, and neurodegeneration.2,3 Nutrient sensing systems have been an intense focus of investigation, including mTOR (the mammalian target of rapamycin) for regulating protein synthesis and cell growth; AMPK (activated protein kinase) for sensing low energy states; and sirtuins, a family of seven proteins critical to DNA expression and aging, which can only function in conjunction with NAD+ (nicotinamide adenine dinucleotide), a coenzyme present in all living cells.4
Across the kingdom of life, an increase in intracellular levels of NAD+ triggers shifts that enhance survival, including boosting energy production and upregulating cellular repair.5 In fact, the slow, ineluctable process of aging has been described as a “cascade of robustness breakdown triggered by a decrease in systemic NAD+ biosynthesis and the resultant functional defects in susceptible organs and tissues.”6 Aging is marked by epigenetic shifts, genomic instability, altered nutrient sensing ability, telomere attrition, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, and dysregulated intercellular communication.7,8
By middle age, our NAD+ levels have plummeted to half that of our youth.9 Numerous studies have demonstrated that boosting NAD+ levels increases insulin sensitivity, reverses mitochondrial dysfunction, and extends lifespan.10,11 NAD+ levels can be increased by activating enzymes that stimulate synthesis of NAD+, by inhibiting an enzyme (CD38) that degrades NAD+, and by supplementing with NAD precursors, including nicotinamide riboside(NR) and nicotinamide mononucleotide (NMN).12,13 A conceptual framework called NAD World, formulated over the last decade by developmental biologist Shin-ichiro Imai, MD, PhD, of Washington University School of Medicine, posits NMN as a critical, systemic signaling molecule that maintains biological robustness of the communication network supporting NAD+.6.