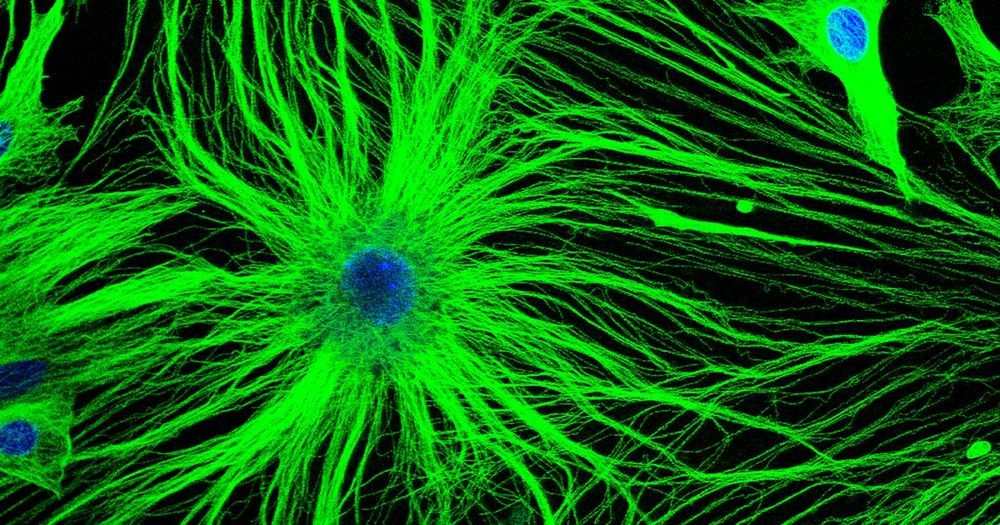
The glial cells of the nervous system have been eclipsed in importance by neurons for decades. But glia are turning out to be central to many neurological functions, including pain perception.
Medical science has been this optimistic before about finding a cure for Alzheimer’s, but in most cases the scientists, patients and their families have suffered serious disappointment. The bitter truth is that over 99 percent of all clinical trials for Alzheimer’s treatments end in failure. For now it is not only incurable, but a major mystery and irreversible. The chemical basis for the disease is still unclear. The research is directed in many directions and based on very different assumptions and approaches.
One focus in recent years is based on the “amyloid assumption,” which says the amyloid beta peptide plays a major role in the development of the disease. The accumulation of the “sticky” amyloid protein plaques is responsible for the damage, by building up into clumps that can cause inflammation in the brain and the death of neurons. These plaques are the main target of most Alzheimer’s research today. Almost 90 percent of the scientific resources in Alzheimer’s research are devoted to developing drugs and treatments to reduce the concentrations and activity of amyloid beta in the brain.

Millions suffer from conditions without known causes. Some contend with constant pain, many live with unrelenting mental anguish. None of them know why.
Now a groundbreaking theory of brain illness — presented in a thrilling new book by science journalist Donna Jackson Nakazawa called “The Angel and the Assassin” (Ballantine Books) — offers big answers by pointing to the tiny packages called microglia.
Microglia are long-dismissed free-floating brain cells located all over the brain, making up 10 percent of the cells that populate the inside of our skulls. According to emerging research, these cells appear to play a significant role in a host of conditions including Parkinson’s disease, schizophrenia, traumatic brain injury, anxiety disorders and more.

New transhumanism and biohacking story out by one of Asia’s most influential newspapers: South China Morning Post:
From brain supplements to chip implants to nootropics, humans are using technology, medicine and extreme diets to improve their brainpower, health and longevity.

Early morning exposure to blue wavelength light can help heal the brain following mild traumatic brain injury (mTBI), new research suggests.
Results of a small, randomized controlled trial showed blue-light therapy improved brain structure and function, cognition, and sleep in this patient population.
“We found that blue-light therapy improved patients’ daytime sleepiness,” study investigator William D. ‘Scott’ Killgore, PhD, told Medscape Medical News. “So those who got the blue light were less sleepy 6 weeks later than they had been at baseline.”

Sometimes, being human involves tragedy: unexpected accidents can alter a person’s future, permanently changing how they need to approach their daily lives. Those with traumatic brain injuries suffer long-term mental and physical challenges, such as trouble with their working memory span, which can play a significant role in their education and longevity. However, if used properly, transhuman aids such as prosthetic limbs can provide solutions to human challenges.
Transhumanism, in a nutshell, is the idea that people can use technology to overcome biological limitations. Just as how we use rational means to improve our life experiences and the world around us, we can use such means to improve ourselves as organisms. It is simply a concept, not a tangible characterization of some futuristic cyborg.
There is reasonable fear that using such technologies would be tampering with nature. This is true. However, whether something is good or bad cannot be decided simply by asking whether or not it is natural. Plenty of natural things are horrible, such as diseases and parasites, where our moral interest is to intervene and improve these conditions. The question to ask is not whether the technology is natural, but rather, what are the various possible consequences that would arise from it, both desirable and undesirable, and the likelihood of each. People who are concerned that our species will stray too far away from what it means to be a ‘natural human’ forget how far we have already evolved as a species.
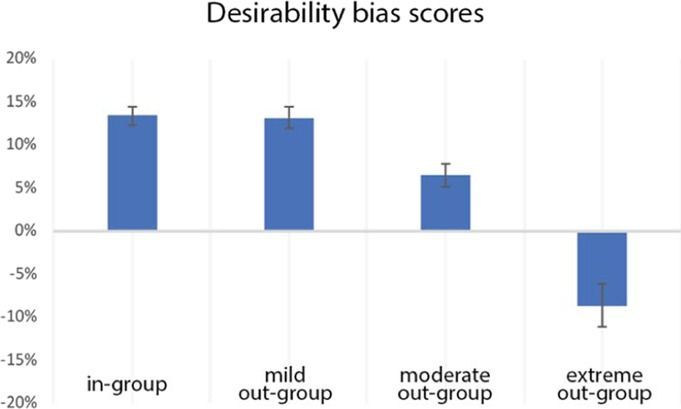
Optimism bias, i.e. expecting the future to hold more desirable than undesirable outcomes, also extends to people that we like or admire. However, it remains unknown how the brain generates this social optimism bias. In this study, respondents estimated the likelihood of future desirable and undesirable outcomes for an in-group and three out-groups: warm-incompetent, cold-competent, and cold-incompetent. We found a strong social optimism bias for the in-group and the warm out-group and an inverted pattern for the cold-incompetent out-group. For all groups, scores of social optimism bias correlated with the brain activity in structures that respondents differentially engaged depending on the target social group. In line with our hypotheses, evaluating the in-group recruited the ventromedial prefrontal cortex and the precuneus/posterior cingulate cortex, whereas evaluating the warm out-group engaged the posterior insula, mid cingulate cortex, and somatosensory cortices. These findings suggest different underlying cognitive mechanisms of social optimism bias for these groups, despite similar behavioural patterns. Thinking about the cold out-groups recruited the right anterior temporal lobe, and temporoparietal junction. Evaluating the cold-incompetent out-group additionally recruited the anterior insula, inferior frontal cortex and dorsomedial frontal cortex. We discuss these neuroimaging findings with respect to their putative cognitive functions.
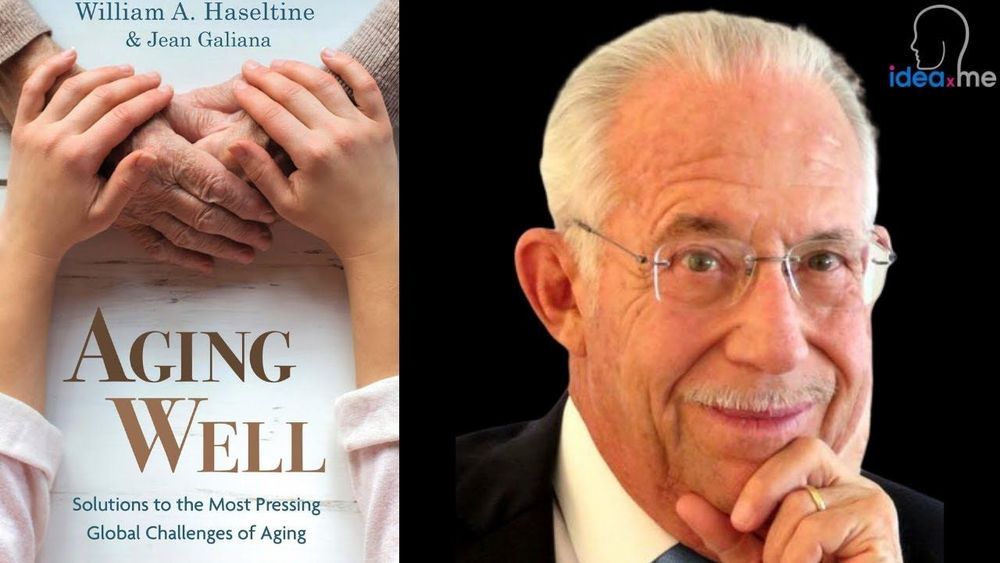
Genomics and BioPharma Pioneer!! — On this ideaXme (http://radioideaxme.com/) episode, I had the honor of being joined by Dr. William Haseltine — biologist, entrepreneur and philanthropist, known for his groundbreaking work on HIV/AIDS and the human genome, now focusing on the issues of healthcare costs, dementia care, and aging — #Ideaxme #Genomics #RegenerativeMedicine #BillHaseltine #Dementia #Biotechnology #Harvard #JamesWatson #WalterGilbert #DavidBaltimore #MIT #CraigVenter #Health #Wellness #Regeneration #Longevity #Aging #IraPastor #Bioquark #Regenerage
Ira Pastor, ideaXme exponential health ambassador, interviews Dr. William Haseltine, American biologist, entrepreneur and philanthropist, known for his groundbreaking work on HIV/AIDS and the human genome.
Ira Pastor Comments:
On today’s show we have a thought leader who sits amongst a rare group of people who have been responsible for creating many aspects of the modern biopharma / genomics / regenerative medicine system as we know it today.
Dr. William Haseltine
Routinely listed in major media sources as one of the world’s most influential business people and most influential leaders in biotechnology, Dr. William Haseltine is an American biologist, entrepreneur and philanthropist, known for his groundbreaking work on HIV/AIDS and the human genome.
Dr. Haseltine earned a PhD in Biophysics at Harvard University, where he worked under the direction of Dr. James Watson, co-discoverer of the structure of DNA, and Dr. Walter Gilbert, Nobel prize winner for developing DNA sequencing techniques.

For the past 10 years, Yale Professors David Spiegel and Jason Crawford have been working on tools to enable the development of glucosepane-cleaving drugs. Kizoo Technology Capital investors say now is the time to advance this groundbreaking research toward the clinic and are leading funding of a new company, Revel Pharmaceuticals Inc., founded by Drs. David Spiegel, Jason Crawford, and Aaron Cravens.
Kizoo leads the seed financing round at Revel, with Oculus co-founder Michael Antonov participating. SENS Research Foundation provided funding to the YaleGlycoSENS group for several years.
The long-lived collagen proteins that give structure to our arteries, skin, and other tissues are continuously exposed to blood sugar and other highly reactive molecules necessary for life. Occasionally, these sugar molecules will bind to collagen and form toxic crosslinks that alter the physical properties of tissues and cause inflammation. As a result, tissues slowly stiffen with aging, leading to rising systolic blood pressure, skin aging, kidney damage, and increased risk of stroke and other damage to the brain.

Stimulating the growth of blood vessels in the brain through the use of fibroblast growth factor 1 (FGF1) may hold promise as a strategy for treating Parkinson’s disease, according to a white paper released by Zhittya Genesis Medicine (ZGM). Clinical trials testing this theory are being planned.
The white paper is titled “Parkinson’s Disease: Therapeutic Angiogenesis as a Disease Modifying, Breakthrough Therapy?”