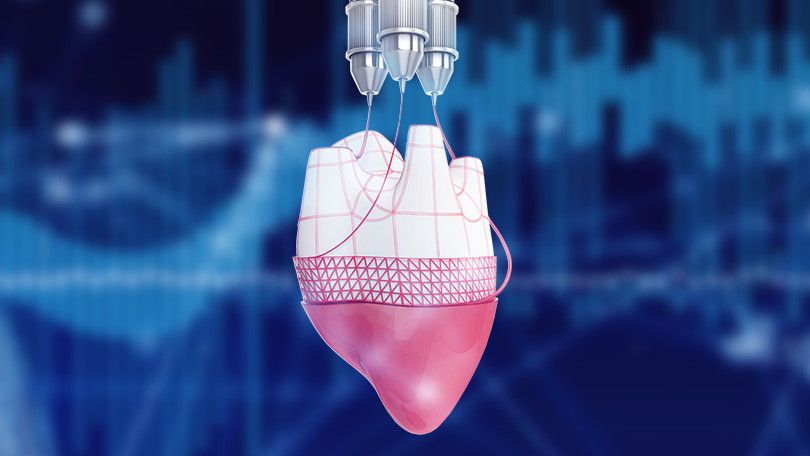
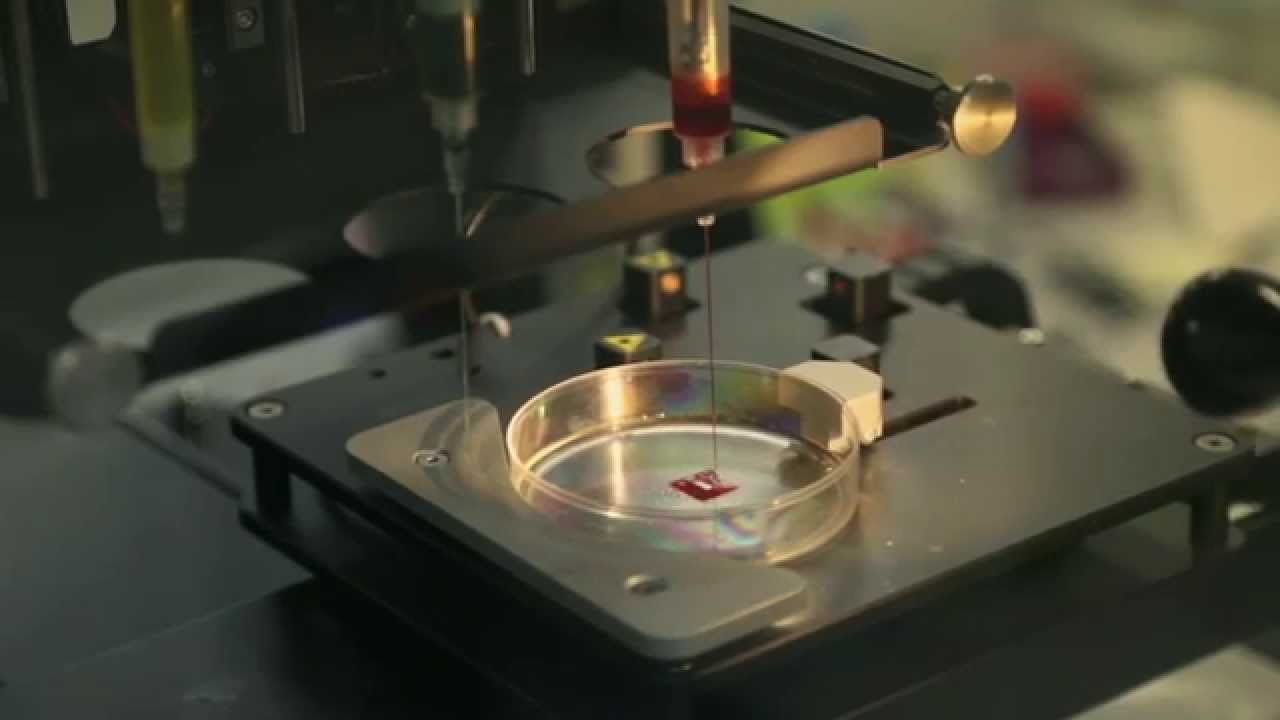
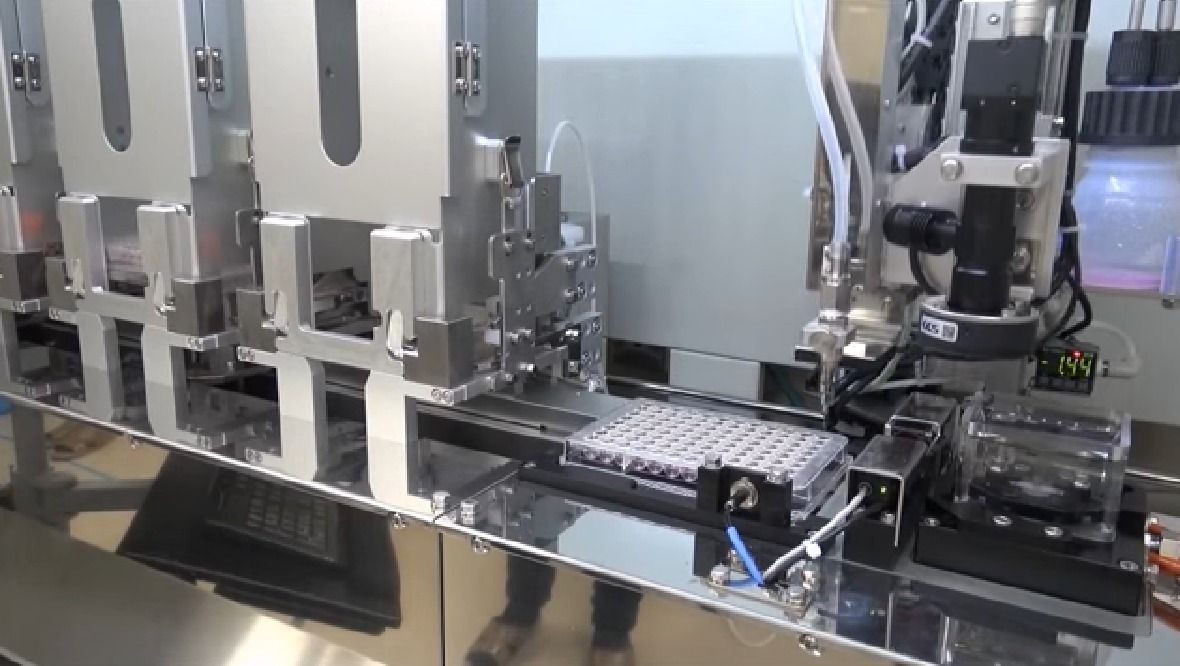
After successfully transplanting the first 3D-printed cornea in an animal, North Carolina company Precise Bio has recently announced the launch of a dedicated business for creating marketable, 3D-printed products for human eyes. Founded by scientists from the Wake Forest Institute of Regenerative Medicine, this company is developing bio-fabrication printers that can restore cells, tissues, and organs. Their proprietary technology, a 4D bio-printing platform, is said to resolve existing limitations presented by other bioprinters to enable more complex tissues to be engineered for transplants and treatments. By focusing on developing marketable products for the eye, the company aims to achieve rapid advancement in its field and move to overhaul the whole organ transplant system.
When a cornea is damaged by disease or injury, a replacement is often needed to restore vision. Transplant surgery using donated corneas is an available solution, however, it relies on a deceased donor. While the waiting list in the United States is nearly non-existent, other countries require longer wait times, some over a year, before one is available. The Eye Bank Association of America estimates that around 10 million people suffer from corneal blindness that could potentially be restored via transplant surgery. An artificially manufactured cornea would overcome supply limitations while also contributing to the knowledge base to develop more complex organs such as hearts and livers.
Read more