The definitive guide to making the Neural Lace a reality.
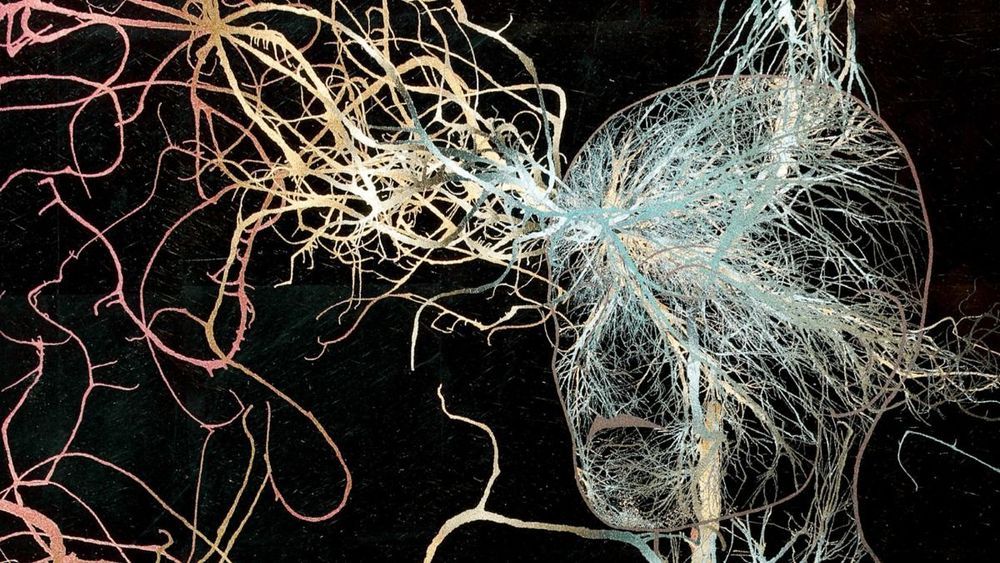
University of Arizona biomedical engineering professor Philipp Gutruf is first author on the paper Fully implantable, optoelectronic systems for battery-free, multimodal operation in neuroscience research, published in Nature Electronics.
Optogenetics is a biological technique that uses light to turn specific neuron groups in the brain on or off. For example, researchers might use optogenetic stimulation to restore movement in case of paralysis or, in the future, to turn off the areas of the brain or spine that cause pain, eliminating the need for—and the increasing dependence on—opioids and other painkillers.
“We’re making these tools to understand how different parts of the brain work,” Gutruf said. “The advantage with optogenetics is that you have cell specificity: You can target specific groups of neurons and investigate their function and relation in the context of the whole brain.”


Environmental cues can trigger powerful memories of substance use. What happens when those memories are disrupted?
01.02.19 5:19 AM ET
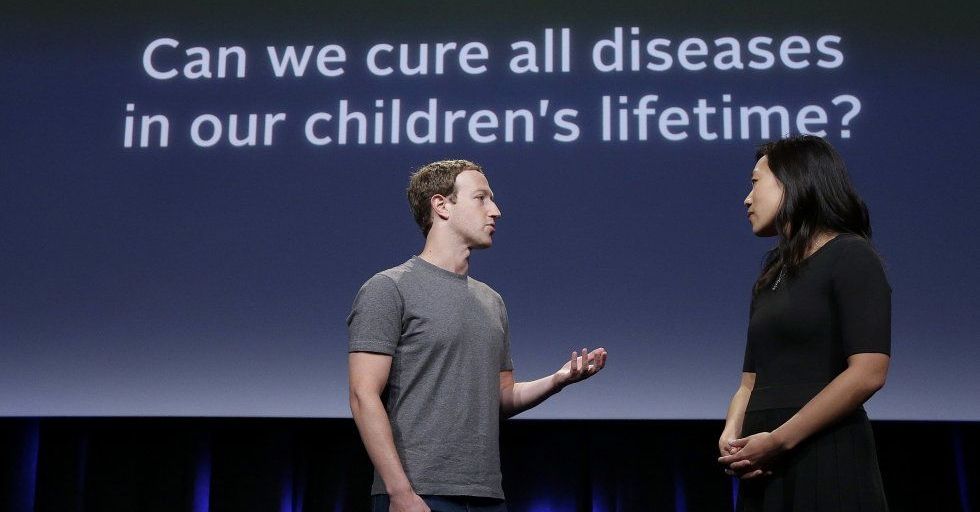
Mark Zuckerberg and his pediatrician wife Priscilla Chan have sold close to 30 million shares of Facebook to fund an ambitious biomedical research project, called the Chan Zuckerberg Initiative (CZI), with a goal of curing all disease within a generation. A less publicized component of that US$5 billion program includes work on brain-machine interfaces, devices that essentially translate thoughts into commands.
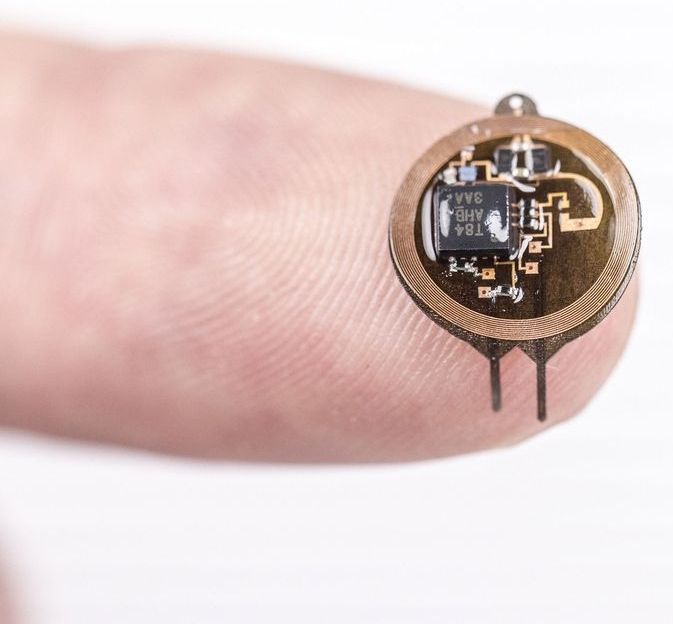
From a report: One recent project is a wireless brain implant that can record, stimulate and disrupt the movement of a monkey in real time. In a paper published in the highly cited scientific journal Nature on Monday, researchers detail a wireless brain device implanted in a primate that records, stimulates, and modifies its brain activity in real time, sensing a normal movement and stopping it immediately. Those researchers are part of the Chan Zuckerberg Biohub, a non-profit medical research group within the CZI. Scientists refer to the interference as “therapy” because it is designed to be used to treat diseases like epilepsy or Parkinson’s by stopping a seizure or other disruptive motion just as it starts.
“Our device is able to monitor the primate’s brain while it’s providing the therapy so you know exactly what’s happening,” Rikky Muller, a co-author of the new study, told Business Insider. A professor of computer science and engineering at the University of California, Berkeley, Muller is also a Biohub investigator. The applications of brain-machine interfaces are far-reaching: while some researchers focus on using them to help assist people with spinal cord injuries or other illnesses that affect movement, others aim to see them transform how everyone interacts with laptops and smartphones. Both a division at Facebook formerly called Building 8 as well as an Elon Musk-founded company called Neuralink have said they are working on the latter.

A ‘pacemaker’ for the brain is on the horizon to prevent people with Parkinson’s and epilepsy suffering from seizures and tremors.
The device is made up of two tiny array of electrodes which sit inside the skull, and link to a circuit board on the side of the head.
The ‘pacemaker’ records the normal electrical current of the brain continually and if it notices a change of rhythm immediately fires a stimulating charge to coax the pulse back to normal.
For several decades now, one of the buzz words in the medical field has been ‘stem cell’. It has been said to aid in treating illnesses like multiple sclerosis, amyotrophic lateral sclerosis, Alzheimer’s disease, and heart diseases.
For the past three years, researchers at the Hubrecht Institute in the Netherlands have been painstakingly cataloging and mapping all the proliferating cells found in mouse hearts, looking for cardiac stem cells. The elusive cells should theoretically be able to repair damaged heart muscle, so the stakes in finding them have been high.
This week, however, Proceedings of the National Academy of Sciences is scheduled to announce the results of the Hubrecht team’s work: no evidence of cardiac stem cells at all.

An injection capable of halting the progress of Alzheimer’s could be available to patients within a decade, Britain’s leading dementia organisation predicts.
The Alzheimer’s Society says a series of recent breakthroughs in treatments that disrupt harmful genes has brought scientists to a “tipping point” in their fight against the disease.
For decades, researchers have sought without success a treatment for Alzheimer’s based on targeting damaging proteins that build up in the brain.
Researchers have explored how memory is tied to the hippocampus, with findings that will expand scientists’ understanding of how memory works and ideally aid in detection, prevention, and treatment of memory disorders.
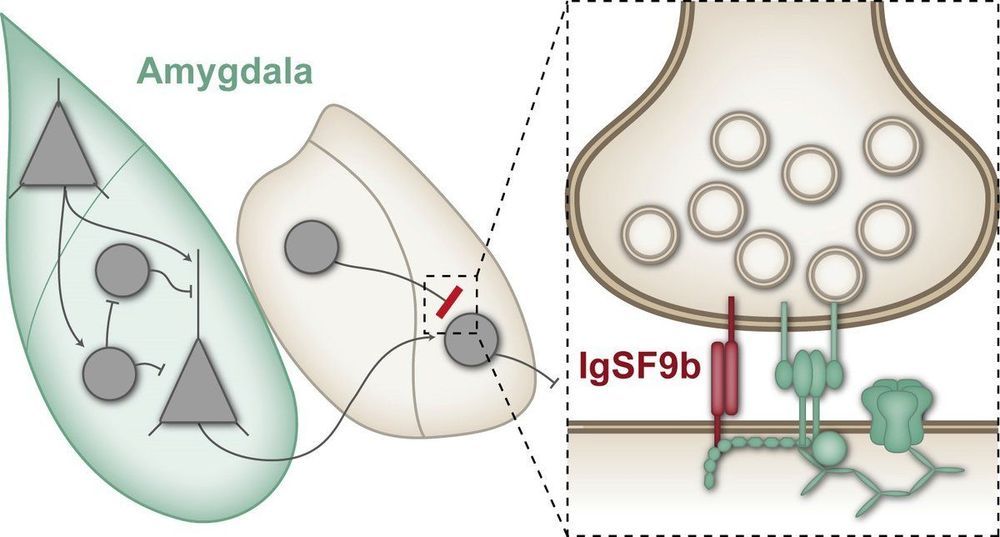
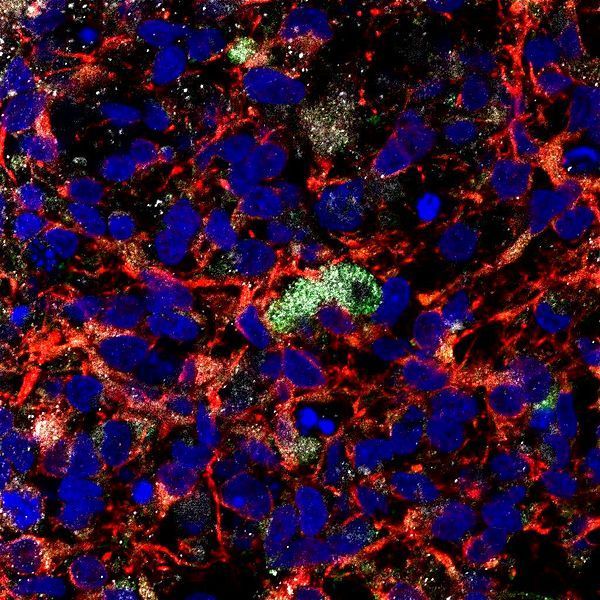
Anxiety disorders are severe mental disorders in which patients suffer from intense fears and anxiety or from sudden, inexplicable panic attacks. In extreme cases, the affected individuals barely leave their homes, which can have serious consequences for their relationships with family and friends as well as for their professional lives. Scientists at the Max Planck Institute for Experimental Medicine in Göttingen have now identified a synaptic protein which, when inactivated, has an anxiolytic effect in mice.
Around 10 percent of the population suffer from anxiety disorders, and current treatment options only offer effective help for a proportion of those affected. One of the changes observed in the brains of patients with anxiety disorders is an increased neuronal activity in the amygdala, a brain region that plays a key role in processing emotions such as anxiety or fear. An overactivation of the amygdala is thought to be involved in causing exaggerated anxiety. Many anxiolytic medications such as benzodiazepines presumably normalize this overactivation by strengthening the function of inhibitory synapses.
Synapses are connections between nerve cells in the brain, at which information is transmitted from one nerve cell to another. At inhibitory synapses, this transmission results in a reduction in the activity of the neighbouring nerve cells. In the amygdala, for instance, this inhibits the transmission of stimuli that trigger fear and anxiety. Benzodiazepines strengthen this inhibitory effect—but unfortunately they affect not only those inhibitory synapses that transmit anxiogenic stimuli but also many other inhibitory synapses in the brain. This can lead to significant side effects such as pronounced sedation and impaired concentration. Accordingly, scientists are searching for new, more specific targets for anxiolytic medications.