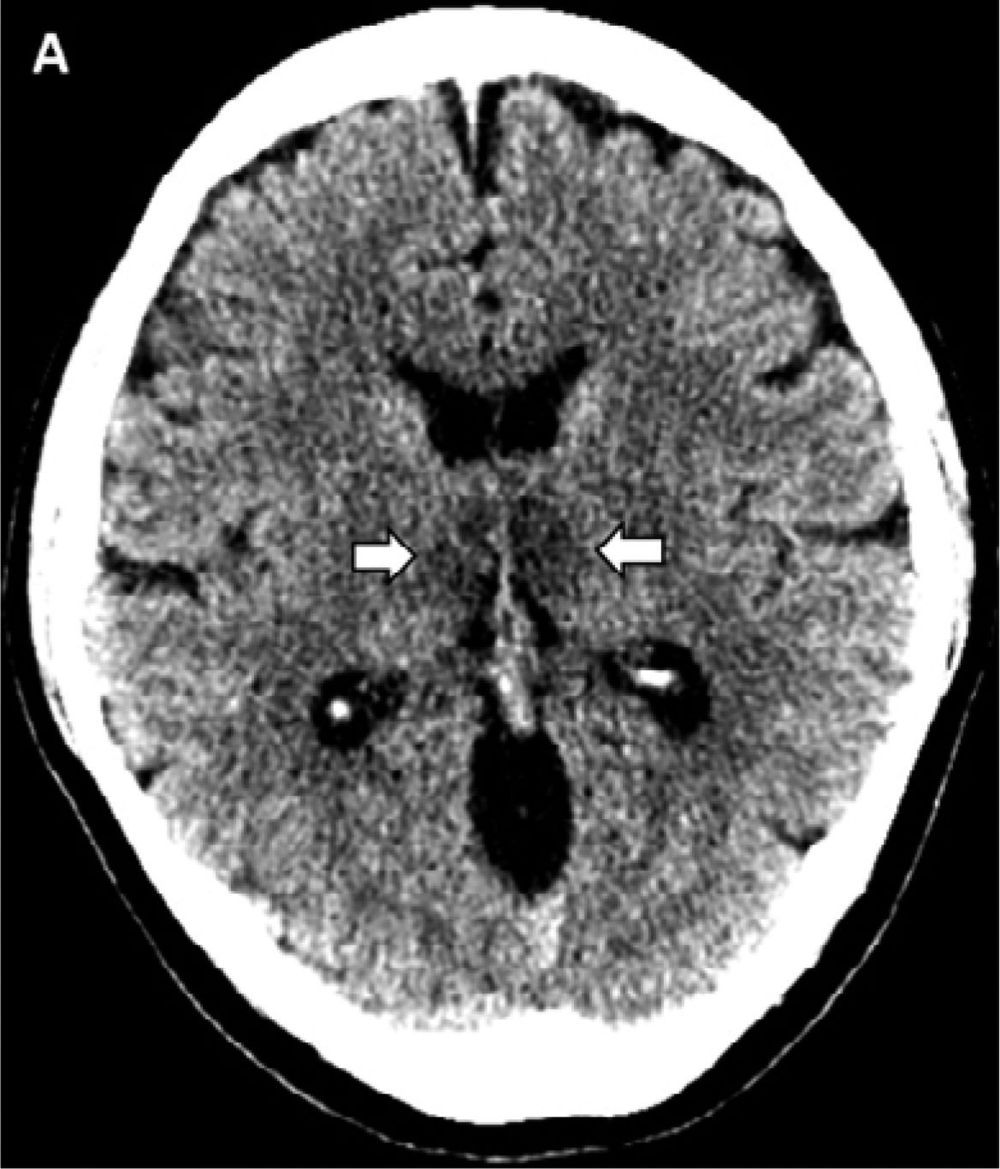
Studies of hibernating animals suggest that the molecular and synaptic integrity of neurons in the cerebral cortex that underlie self and consciousness is maintained in many cases when from the outside the brain appears dead.
A striking feature of medicine over the past few centuries has been our growing ability to bring people back from the “dead.” For most of human history, patients who were unconscious and not breathing were treated as though they had died. But the concept of resuscitation emerged as doctors grew to understand the basic function of the lungs and airways. That led to new techniques and tools capable of restoring both breathing and heartbeat — and the realization that cardiac arrest was not always a death sentence. That, in turn, gave rise to a distinction between what’s now called clinical death versus brain death.
Today that brain focus continues, but with a growing glimmer of hope that even brain death might be reversible in some instances. These dreams are fueled by research showing that the disappearance of brain function is not the same as deletion of computer files. Rather, it represents a deterioration of the pathways that normally enable different parts of the brain to communicate. This idea was bolstered recently with the 2017 success in France, where a patient was partially revived from a 15-year vegetative state. It also dovetails with insights from the study of hibernating animals.
Medical magic: Expansion of resuscitation of capability over the centuries
Resuscitation entered the field of medicine beginning in the 1500s, not surprisingly with practices that may have helped victims occasionally, but with a low success rate. Such practices included flagellation, and were based on experience rather than an understanding of the underlying physiological processes. This started to change with the use of air bellows, based on an understanding that air needed to flow in and out of the lungs. But the 1740s, mouth-to-mouth resuscitation was standard practice in France for resuscitating drowning victims.