A woman in her forties has become the latest known case of SARS-CoV-2 infection associated with a “sudden and complete” loss of smell. Known as anosmia, loss of smell is regarded as one of the tell-tale signs of COVID-19.
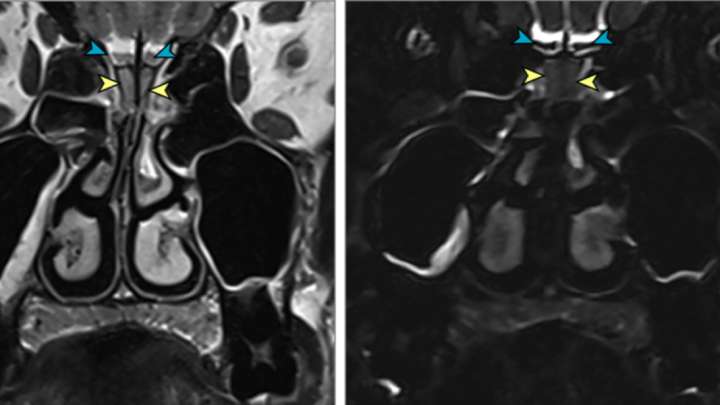
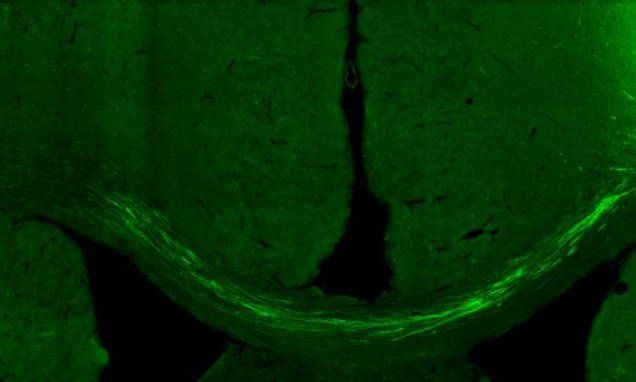
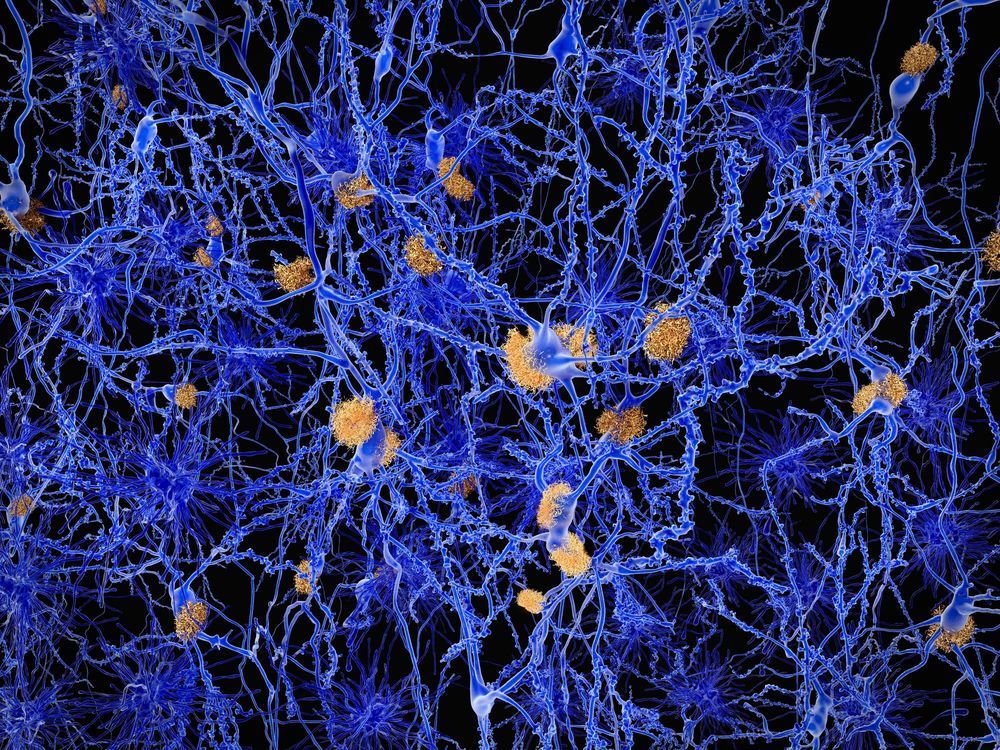
When an odor enters the nose, neurons in the nasal cavity send messages to the olfactory bulb, a structure in the front part of the brain. These signals are then shipped off to different parts of the brain, leading some medical experts to wonder whether the novel coronavirus could cause adverse neurological reactions.
But how could a virus associated with respiratory infections impact the brain? Researchers are trying to find out. Dr Serena Spudich, a neurologist at the Yale School of Medicine specializing in infectious diseases, says that it is too early to say definitively whether SARS-CoV-2 directly infects the brain but limited data suggests it is a possibility.