“Like you often have to do in science, we first hit the problem with a hammer to see how the system breaks, then backtrack from there,” Simpson said.
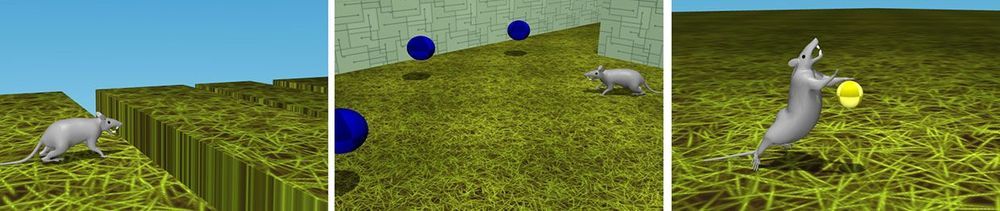
By that she means that in order to determine if the gut microbiome influenced drug addiction, they first needed to compare an organism with a normal gut microbiome to one without. To do that, the researchers gave some rats antibiotics that depleted 80 percent of their gut microbes. All of the rats — those with and without gut microbes — were dependent on the prescription opioid pain reliever oxycodone. Then some of the rats from each group went into withdrawal.
“To me, the most surprising thing was that the rats all seemed the same on the surface,” George said. “There weren’t any major changes in the pain-relieving effect of opioids, or symptoms of withdrawal or other behavior between the rats with and without gut microbes.”
It wasn’t until the team looked at the rats’ brains that they saw a significant difference. The typical pattern of neuron recruitment to different parts of the brain during intoxication and withdrawal was disrupted in rats that had been treated with antibiotics, and thus lacked most of their gut microbes. Most notably, during intoxication, rats with depleted gut microbes had more activated neurons in the regions of the brain that regulate stress and pain (periaqueductal gray, locus coeruleus) and regions involved in opioid intoxication and withdrawal (central amygdala, basolateral amygdala). During withdrawal, microbe-depleted rats had fewer activated neurons in the central amygdala, as compared to rats with normal gut microbiomes.
“It was many months of counting black dots,” Simpson said. “But in the end it became clear that, at least in rats, gut microbes alter the way the brain responds to drugs.”
That shift could affect behavior, she explained, because a decrease in neurons recruited in the central amygdala could result in fewer withdrawal symptoms, which can in turn lead to a higher risk of drug abuse.
As a now-healthy graduate student, Simpson first worked on techniques to visualize molecules in the brain. But she couldn’t shake her interest in the gut microbiome and its connections to the brain.
“So one day, Sierra just walks into my lab and asks me if I’d be interested in exploring potential connections between the gut microbiome and what my lab typically studies — drug abuse and addiction,” said Olivier George, PhD, associate professor of psychiatry at University of California San Diego School of Medicine. “I was reluctant at first. After all, I figured if there was something there, someone would’ve discovered it by now. But we decided to give it a try.”
In a study published April 27, 2020 in eNeuro, Simpson, George and team discovered that the gut microbiome influences the pattern of activation in a rat’s brain during opioid addiction and withdrawal.