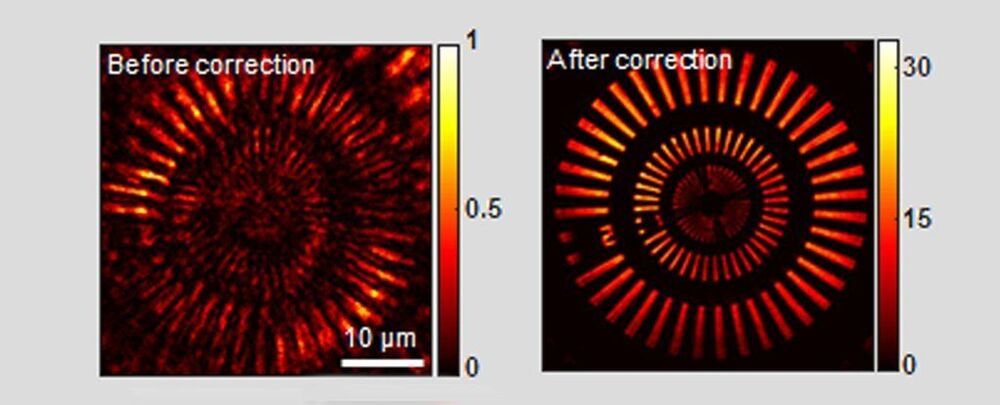
Just a few doses of an experimental drug can reverse age-related declines in memory and mental flexibility in mice, according to a new study by UC San Francisco scientists. The drug, called ISRIB, has already been shown in laboratory studies to restore memory function months after traumatic brain injury (TBI), reverse cognitive impairments in Down Syndrome, prevent noise-related hearing loss, fight certain types of prostate cancer, and even enhance cognition in healthy animals.
In the new study, published Dec. 1, 2020, in the open-access journal eLife, researchers showed rapid restoration of youthful cognitive abilities in aged mice, accompanied by a rejuvenation of brain and immune cells that could help explain improvements in brain function.
“ISRIB’s extremely rapid effects show for the first time that a significant component of age-related cognitive losses may be caused by a kind of reversible physiological “blockage” rather than more permanent degradation,” said Susanna Rosi, PhD, Lewis and Ruth Cozen Chair II and professor in the departments of Neurological Surgery and of Physical Therapy and Rehabilitation Science.