I learn useful life lessons from each patient I meet. Some are positive messages, reminding me of the importance of maintaining balance between family, work, and leisure activities, but more frequently I witness examples of the remarkable resilience of the human spirit when facing the reality and risks of a major surgical procedure and a diagnosis of cancer. Rarely, patients and their family members utter remorseful or simply sad remarks when they are faced with a grim prognosis and the emotions associated with an onrushing date with mortality. These comments invariably involve an inventory of regrets in life, including, “I should have spent more time with my kids,” “I wish I had told my father (or mother, brother, sister, child, or some other person) that I loved them before they died,” and “I have spent my entire life working, I never took time for anything else.” I wince when I hear these openly expressed remonstrations, I recognize that I am hearing painful and heartfelt truths. Not a week goes by that I am not reminded that I do not one day want to look back at my life with a long list of regrets, should have dones, and what ifs.
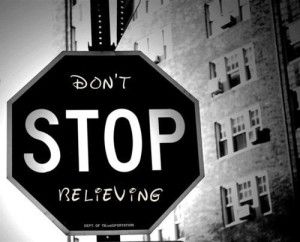
I was blessed to meet a great teacher in the guise of a patient early in my academic career. He came to my clinic in my first year after completing a Fellowship in Surgical Oncology, my first year as an Assistant Professor of Surgery. My patient was a 69 year-old Baptist Minister from a small town in Mississippi. He was referred to me by his medical oncologist who called me and said, “I don’t think there is anything you can do for him, but he needs to hear that from you because he doesn’t believe me.” This tall, imposing man had colon cancer that had metastasized (spread) to his liver. The malignant tumor in his colon was removed the year before I met him, and he had received chemotherapy to treat several large tumors found in his liver. The chemotherapy had not worked and the tumors grew. At the point I met him, the medical oncologist told him he would live no more than 6 months, and because he was an avid fisherman when not preaching or helping others in his community , the doctor suggested that he go out and enjoy his remaining time by getting in as much fishing as possible. I learned two invaluable lessons from this patient and his family. First, never deny or dismiss hope from a patient or their family, even when from a medical perspective the situation seems hopeless and the patient is incurable. Second, quoting the minister directly, “Some doctors think of themselves as gods with a small ‘g’, but not one of you is God”.
When I first walked into the examining room, this man was slouched on the examining table in the perfunctory blue and white, open-backed, always unflattering hospital gown. He made eye contact with me briefly, then looked down to the floor. In that momentary meeting of our eyes, I saw no sparkle, no life, no hope in his eyes. He responded to my initial questions with a monotonic and quiet voice. Several times I had to ask him to repeat an answer because his response was so muted. Mid-way through our first visit, the patient’s wife told me he had been very depressed by his diagnosis of untreatable metastatic colon cancer. She reported, despite his occasional side-long warning glances requesting her silence, that while he was eating well, he was spending most of his time sitting in a chair or laying in bed, and that the active, gregarious man with the quick wit and booming voice she had married was gone.
After I interviewed and examined the Minister I left the room so he could dress and sit in a chair next to his wife. I reviewed the results of the lab tests and CT scans we had performed on him, and then returned to the examining room. I explained to them that I believed it was possible to perform a difficult operation that would remove approximately 80% of his liver. The operation would be risky, it was possible he would require blood transfusions, and as a worst-case scenario the small amount of remaining liver might not be sufficient to perform necessary functions. If I pushed the surgical envelope too far and removed too much normal liver, following the operation he could develop liver failure leading rapidly to his death. I also stated, assuming he survived a major operation and the recovery period, that I could not predict his long-term outcome or survival. I emphasized that even if the operation was successful, it was possible that the cancer would recur in the remaining liver or in some other organ. I even attempted to raise his spirits a bit by injecting some puerile surgical word play when I said, “This operation will leave you with little more than a sliver of liver, but God willing it will be enough!” At the conclusion of my very direct monologue, he looked up from the floor and once again his eyes met mine. I remember blinking several times in surprise at how different his eyes now appeared. With his eyes bright and twinkling he asked, “Are you saying there is hope?” I replied that I believed there was hope, albeit small and impossible to measure, but hope nonetheless. An unforgettable and immediate transformation occurred in his demeanor and as his wife smiled at me and mouthed the words, “He’s back”; he reverted instantaneously to what I would come to learn was his former garrulous self.
The spiritually-resuscitated Minister sat upright, grasped my right hand with both of his hands, and launched into a memorable diatribe. “Never deny someone hope doctor, no matter how hopeless you know the situation to be. Humans need hope, without it comes depression, despair, and death. Why do you think the Jewish defenders at Masada held out against an overwhelming Roman force for so long? Because they had hope, and they had faith. Why do people let you cut them open? Hope. Never deny a human being hope doctor, without it we have no humanity, we are only another animal.” He was a forceful and eloquent speaker. With his Mississippi drawl, he could alternatively be plain spoken or pedantic. He was a well-read and educated man and he loved to display his extensive etymologic armamentarium. Not infrequently after our conversations I would seek out a dictionary to learn the meaning of a word or two. I had no difficulty visualizing him preaching from a pulpit in his Baptist church, like a yo-yo dropping his parishioners to the floor with the fear of eternal damnation, and then pulling them back up into his hands with a message of redemption and salvation.
I walked out of the examination room enthralled and scheduled the operation for the next week. I was amazed by the sudden change I had witnessed in this man’s posture and overall demeanor. As with all who provide care for patients with debilitating and serious medical conditions, I have seen patients lapse into a state of abject, deep despair and complete hopelessness. Like an autumn leaf falling from a tree branch, their spiritual demise leads to a rapid downward spiral of their physical condition. These patients fulfill the expectations of medical practitioners who have told them their survival will be a matter of only weeks or months, in fact I have seen several patients die much more rapidly than I would have predicted when darkness and despair overwhelmed them.
I had the Minister’s “sermon” on my mind throughout his operation. As I expected, the operation was technically difficult. He was a robust, barrel-chested man and had four large tumors in his liver. Two of these were right lobe of the liver only, but the other two extended from the right lobe of his liver into portions of the left lobe of the liver. One of these latter two tumors also extended down to involve two of the three large veins that drain blood from the liver into the large vein, called the inferior vena cava, that carries blood back to the heart. To assure that I had completely removed all of the tumor around these two veins, I removed a portion of the wall of the inferior vena cava and replaced it with a patch from another vein. It was a liver surgery tour-de-force, and at the conclusion of the operation the surgical fellow who performed the operation with me and I quietly congratulated one another on a job well done. Nonetheless, I admit to my own negative sentiments and relative paucity of optimism at the end of the operation. I remarked to the surgical fellow working with me that while the operation had been technically challenging and a great lesson in surgical anatomy, I doubted that we had cured this patient because I was concerned his aggressive cancer would return.
“Never deny someone hope doctor.” If I ever had a crystal ball to predict the future, I obviously dropped it in the mud a long time ago. I was wrong about the Minister. His cancer never returned. He spent only one week in the hospital after his operation and his sliver of liver performed and regenerated beautifully. For the first five years after the operation I saw him every three to six months with lab tests and CT scans to check for return of malignant tumors. For the next six years I saw him only for an annual visit. This man survived and enjoyed life for eleven years after being told that he only had only six months to live. He died as many of us would wish to die, in his sleep from a stroke. He gave his last sermon from the pulpit of his church three days before he died. His cancer never returned to prey upon his mind and hunt down his hope.
After thinking about it, I realize I learned one additional lesson from this patient. He taught me that it was acceptable to express a little clean, righteous anger and then laugh and move on. The Minister and I developed a ritual that was repeated with each of his visits after passage of the initial six months he was told he would live by his medical oncologist. After I reviewed the results of his tests and CT scans and confirmed that all was well and that cancer had not returned, he would smile and say, “Let’s do it!” From the examining room, I would dial the phone number of the medical oncologist in Mississippi who had referred him to me. The Minister admitted to me he was angry that this doctor had needlessly denied him hope. When the medical oncologist came to the phone, I would hand it to the Minister, who would identify himself to the doctor, and then he would say the same exact words, “Hey doc, you want to go fishing?” As a surgeon, I confess I enjoyed witnessing the surgical precision with which the preacher inserted this verbal blade, deftly turning it to maximize the impact of his statement. When I passed the phone to the Minister, he always had an impish, perhaps even devilish grin on his face. Each time after he asked the doctor in Mississippi if he would care to join him for a fishing expedition, he would hand the phone back to me and a look of beatific serenity would come to his face. The ritual was completed when I would take the phone and speak to the doctor in Mississippi. In my first few conversations with this physician, I apologized for my obvious and indecorous breach in professional behavior, but to the credit of this man being regularly taunted by a Baptist Minister who wasn’t entirely forgiving, he would tell me that no apology was necessary and that he believed he deserved and benefited from these brief but poignant verbal reminders. As the years passed, he would be laughing when I put the phone to my ear and tell me that he really enjoyed those calls and that his whole office staff looked forward to this annual event.
Two years before the Minister finally died at the age of 80, the doctor in Mississippi told me that because of this patient, he never answered the question asked to him by patients about their expected longevity with a diagnosis of advanced cancer. Instead, he would inform the patients and their families that he really couldn’t make such a prediction because of marked individual differences in responses to treatment, along with the immeasurable will to live even in individuals no longer receiving treatment for their cancer. Together, he and I learned the importance of leaving no treatment stone unturned; to engage in multidisciplinary management and to consider all options for our patients. Great lessons from a great spiritual teacher, taught to a couple of hard-headed doctors.
“Hey doc, you want to go fishing?”