Glycerol, used in the past as antifreeze for cars, is produced by a range of organisms from yeasts to vertebrates, some of which use it as an osmoprotectant—a molecule that prevents dangerous water loss in salty environments—while others use it as an antifreeze. Here, scientists from the University of Nevada and Miami University in Ohio show that two species of the single-celled green algae Chlamydomonas from Antarctica, called UWO241 and ICE-MDV, produce high levels of glycerol to protect them from osmotic water loss, and possibly also from freezing injury. Presently, only one other organism, an Arctic fish, is known to use glycerol for both purposes. Both species synthesize glycerol with enzymes encoded by multiple copies of a recently discovered ancient gene family. These results, published today in the open-access journal Frontiers in Plant Science, illustrate the importance of adaptations that allow life to not only survive but to thrive in extreme habitats.
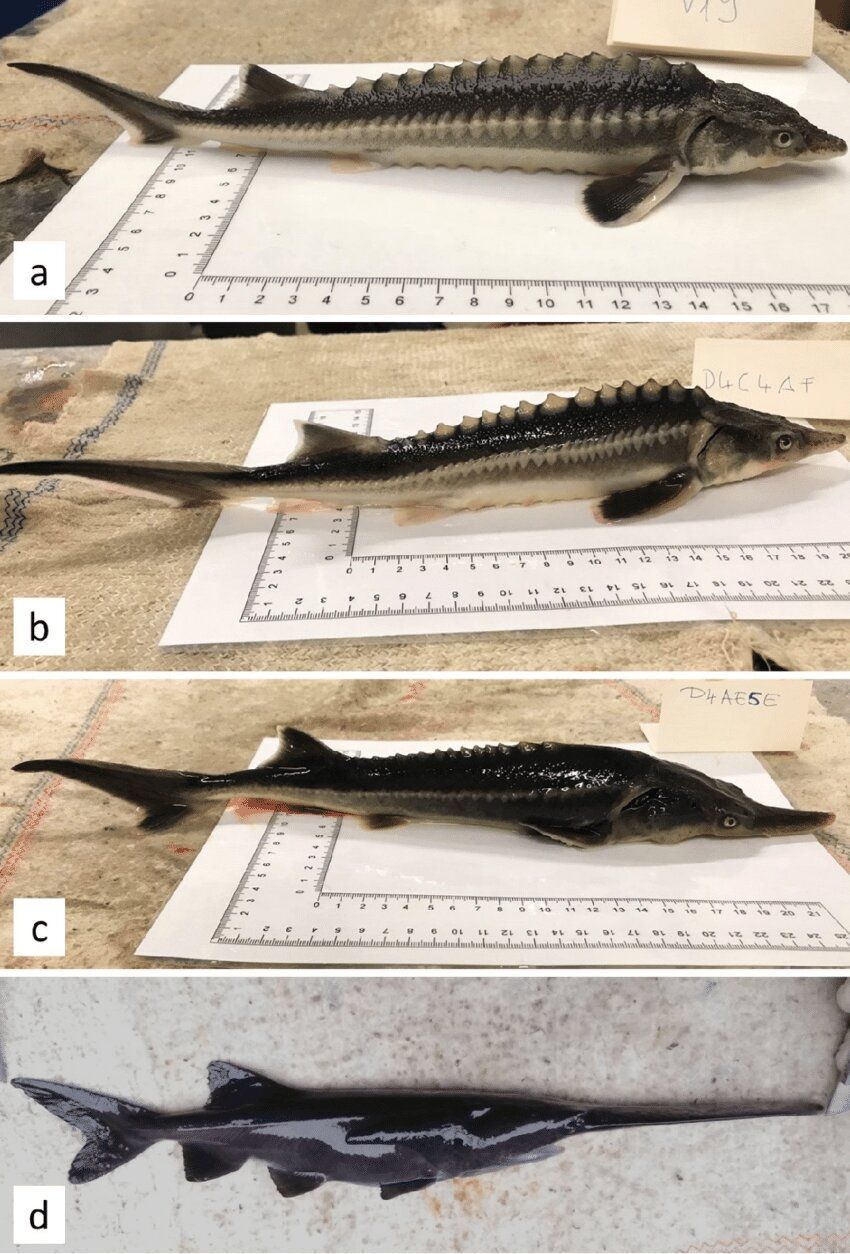
The researchers collected both Chlamydomonas species from depths of 13 to 17 m, a region with a steep salinity gradient, in Lake Bonney, a permanently ice-covered lake in the McMurdo Dry Valleys of Victoria Land, Antarctica. Previously, they showed that both species are remarkably adapted to their extreme habitat, with a photosynthetic apparatus adapted to cold, saline, and light-poor conditions, novel proteins, more fluid cell membranes that function at low temperatures, and ice-binding proteins that protect against freeze-thaw injury.
“Our overall goal is to understand how microorganisms survive in extreme environments. The Chlamydomonas species of Lake Bonney are well-suited for such studies because they are exposed to many extremes, including low light, low temperature, oxidative stress, and high salinity. The present results are the first to show that glycerol production by microorganisms, which is well-known in warm, salty environments, is also important in polar regions,” says corresponding author Dr. James Raymond, Adjunct Research Professor at the School of Life Sciences, University of Nevada, Las Vegas, USA.