Dr Michael Fossel is a PhD and MD heading up telomerase research and therapy and has kindly written a blog article for Bioviva detailing the work both they and his company Telocyte are doing to fight back against Alzheimer’s.
How Alzheimer’s Can Be Prevented and Cured…
Michael Fossel, MD, PhD
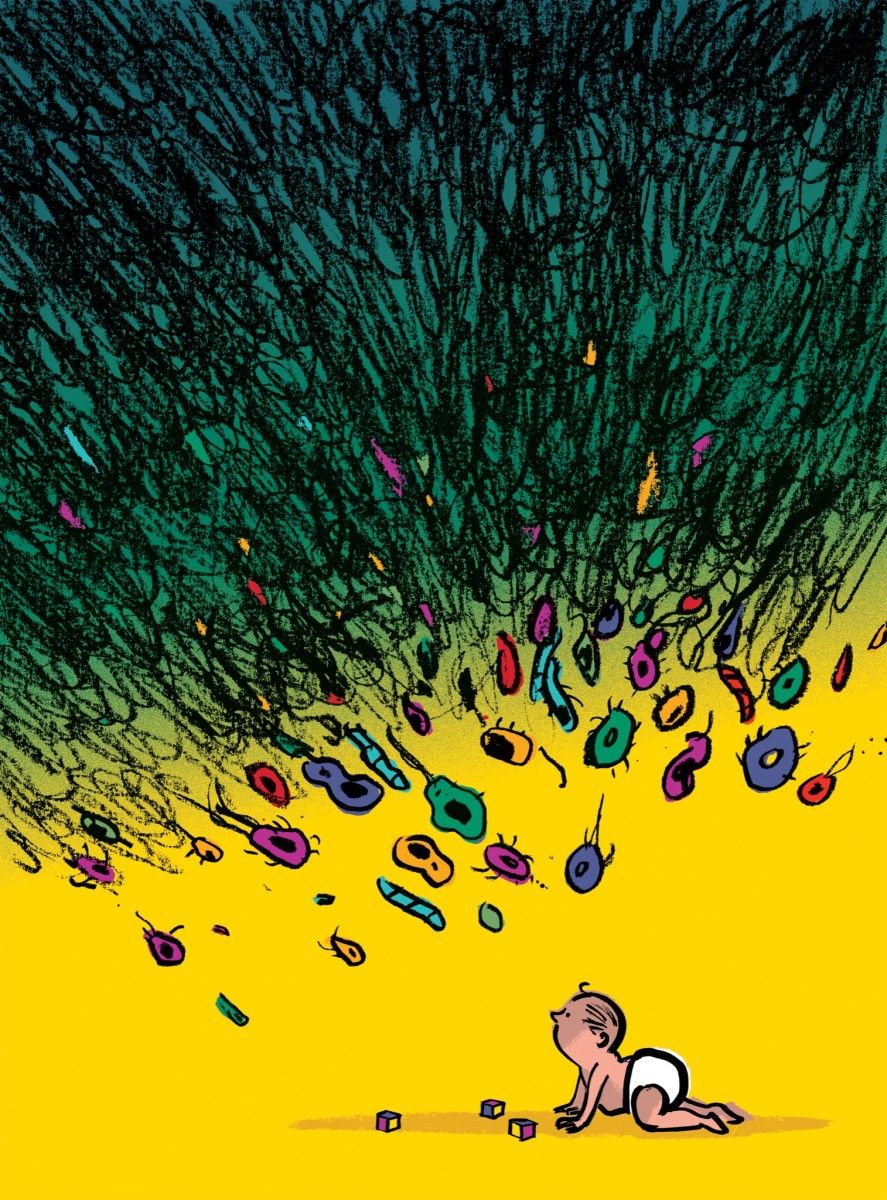
As I said in my medical textbook on aging, “If age is a thief, then the greatest treasure we lose is ourselves.” We fear Alzheimer’s not simply because it takes away our health, but because it steals our souls.
Once, we thought it was simply “old age” that gradually killed the cells that carry information and memory. These are brain cells that make us who we are and define our consciousness.
Only in the past two decades, have we gradually come to realize that it’s not the neurons, which are merely the innocent bystanders in the tragedy,
but the microglial cells that cause the disease. It’s our microglia, not our neurons that steal our very souls.
Alzheimer’s disease begins in our glial cells. These cells together form.
90% of our brains, while neurons are only a small minority in the nervous system.
One set of these glial cells, the microglia, have the critical job of protecting the neurons and supporting them metabolically. These are the cells that, among dozens of other functions, are responsible for clearing metabolic waste products and recycling the extracellular proteins that surround the neurons.
Unfortunately, as we age, the microglial cells not only fail to divide, but gradually lose telomere length. By itself, telomere loss is unimportant,
but this loss begins a cascade of crucial changes in our cells.
As these telomeres shorten, they trigger a gradual shift in gene expression throughout the entire microglial cell. While the genes remain unchanged,
the “tune they play” i.e. the epigenetic pattern of gene expression becomes a sinister song. Proteins that are critical to DNA repair, to making our mitochondria work, to holding free radical damage to a minimum, begin to become scant. Where once, a young microglial cell would recycle proteins quickly and efficiently– including beta amyloid proteins — as the cell ages, the rate of turnover slows to a crawl.
The problem is much like many other things in life. If cell phones were replaced not every two years, but every twenty years, few of them would work. If a garden is weeded not every week, but once every two years, it would be engulfed in weeds. If we showered not once a day, but once every year, few of us would have friends.
Cells are no different: if we recycle proteins quickly, there is little damage, but if we recycle proteins slowly, then the damage begins to become obvious. Our cells don’t age because they are damaged; rather our cells permit damage to accumulate because they age. Shorter telomeres cause changes in gene expression, slower cell recycling, with the end results being old, damaged cells.
In Alzheimer’s disease, the microglia is the earliest change, the key change that begins the entire cascade of pathology to dementia. As our microglial cells slow down, they no longer keep up with the damage around them and the result is a gradual accumulation of damaged and denatured proteins.
The disaster begins.
At first, only trivial amounts of beta amyloid begin to accumulate in small aggregates, but then they grow larger, gathering into huge amyloid plaques.
Where once they could barely be seen, they now become visible under a microscope. But the problem is not simply these plaques themselves, but their effect on the neurons. Beta amyloid protein is critical to cell function, but only in small amounts, not in the vast plaques that now surround the besieged neuron. These growing plaques are toxic to neurons,
making it harder and harder for these cells to survive, let alone function normally.
Tau proteins likewise begin to form tangles and the neurons can no longer maintain themselves. At first, they begin to lose the ability to transmit nerve impulses, then they become more and more damaged internally, until the neurons die, first only a few, then in larger populations, leaving only scars, inflammation, and empty space. One-by-one our neurons are snuffed out, submerged under the rising effects of beta amyloid and tau proteins,
and all of this, the plaques, the tangles, and the dying neurons characteristic of Alzheimer’s can be traced back to the failing microglial cells.
As I write this, there have been more than 1,300 clinical Alzheimer’s trials looking at potential interventions. Many deal only with nursing care, but of those that try to intervene in the actual pathology, most have amyloid as their target, and a few target tau proteins. Small wonder then,
that none of these trials has ever been able to slow, let alone stop, or even reverse the disease. Every one of them is aimed at the wrong target.
Instead of trying to reverse the primary problem — the changes within the aging microglial cell — they aim at what are merely symptoms and results rather than causes. Imagine what would happen if we tried to cure bacterial infections by aiming merely at fevers, rather than aiming at the bacterial themselves. Current clinical trials are much the same: instead of aiming at the cause, they aim at the result.
Can we do better?
Almost certainly, we can. We know that the changes in gene expression that define aging in our cells are controlled by the changing telomere lengths as these cells divide.
We also know that if we reset the telomere to the original length, we not only reset gene expression, but end up with a cell that looks and acts like a young cell.
We have even done this not only in human tissues, in the lab, but in animals such as mice and rats. When we reset telomere lengths in the aging rodent brain, the animals begin to act normally again and we see the brains returning toward normal volume and function.
Can we do the same for human patients? Can we cure Alzheimer’s disease? We almost certainly can. We now not only understand how the disease works, and we not only have been able to show we can manage to intervene in animals,
but we already have the tools we need to cure Alzheimer’s disease in those we love.
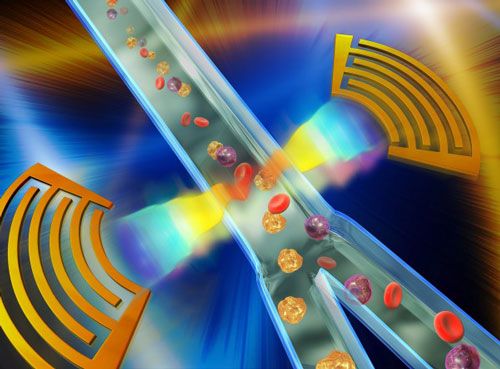
Telomeres can be reset using telomerase, and enzymes comprising hTERT and hTERC. hTERT stands for human telomerase reverse transcriptase. hTERC
stands for human telomerase RNA component. Both of these telomere length extending enzymes can be delivered into the human brain, using either liposomes or viral vectors, much as has already been done in animal trials.
Once we can reverse the disease, once we can cure Alzheimer’s, it will change from the most frightening of illnesses to one we can deal with:
easily prevented, easily cured, and (much as it once erased our personal memories) a forgotten thing of the past.
There are at least two biotech projects currently aimed at human trials,
one via standard FDA-sponsored research (Telocyte), the other using a faster and less formal, “offshore” approach (BioViva). We support both approaches, wanting an effective therapy for Alzheimer’s that is both safe and rapidly available to all.
BioViva is seeking funding to initiate the use of these kinds of microglial telomere lengthening therapies in human test subjects immediately. If successful, we might not just eradicate Alzheimer’s disease, but also the cognitive impairment that strikes all people as they age past 30.
Maximum Life Foundation is raising $250,000 to give a grant to BioViva to test these therapies on human volunteers. 100% of donations earmarked for this study will be sent to BioViva with nothing subtracted for overhead.
The grant would cover this initial phase of the study and more.
To make your tax-deductible donation to this special fund aimed at quickly testing these telomere lengthening approaches in aging humans, go to www. MaxLife.org, or send your check to:
Maximum Life Foundation (BioViva)
2324 Colony Plaza Newport Beach,
CA 92660
Tele: (800) 881‑5346.
Read more