“How would you like to be known as the neurosurgeon who cured Parkinson’s disease?”
A month before the scheduled surgery, the four researchers were ready to chaperone the brain cells on their 190-mile journey. They never anticipated they were in for “The Amazing Race”-meets-“ER.”
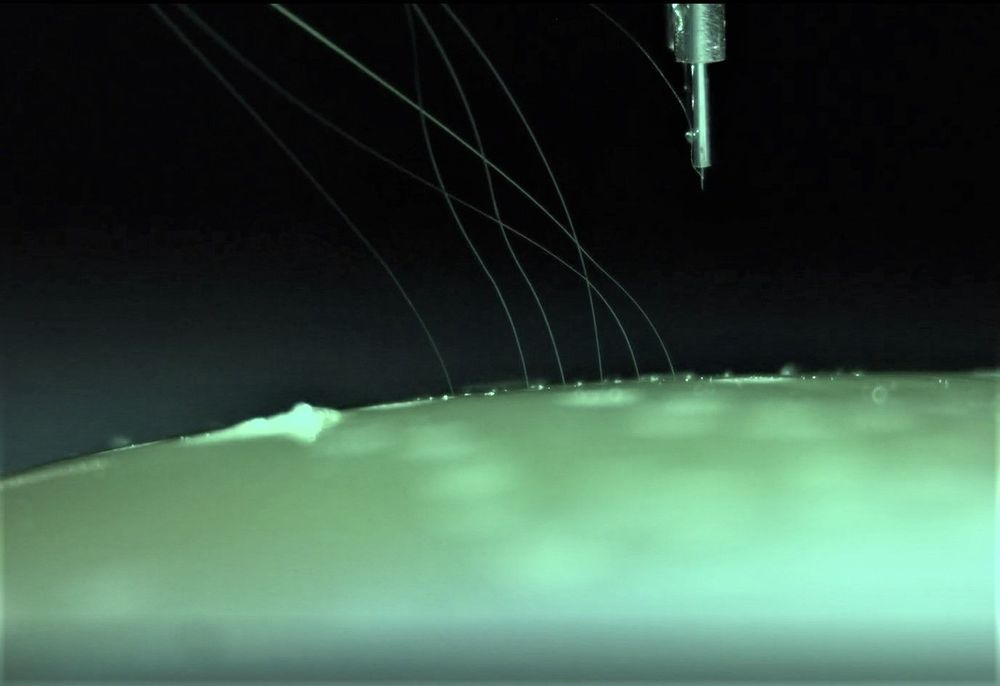
It was after midnight on a late summer night in 2017, and they had less than eight hours to get the cells by ambulance, private plane, and another ambulance from Dana-Farber Cancer Institute in Boston to Weill Cornell Medical Center in Manhattan. If it took longer, the cells would almost certainly be DOA, and so might the researchers’ plan to carry out an experimental transplant surgery unprecedented in the annals of medicine: replacing the dysfunctional brain cells of a Parkinson’s disease patient with the progeny of an extraordinary type of stem cell. Created in the lab from a patch of the patient’s own skin, these cells, it was hoped, would settle into the brain like they belonged there and permanently restore the patient’s ability to walk and move normally.
If successful, the surgery could forever change Parkinson’s disease, from an inexorable, cruel, and sometimes fatal decline to — for at least some patients — a condition that can be successfully treated.