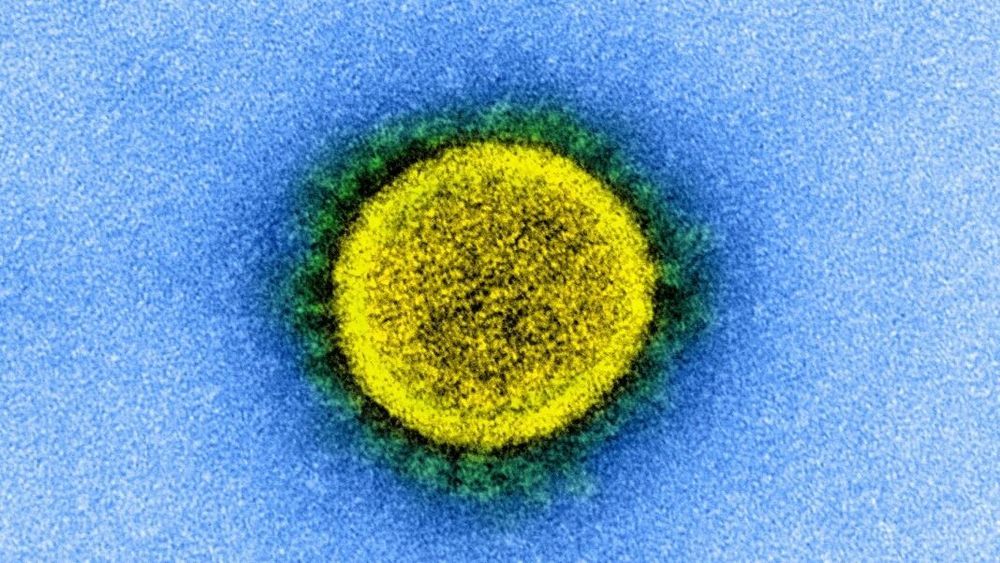
This is very surreal. A study was done to assess the safety of common drugs, and COVID, and whether taking them leads to severe symptoms. There has been concern as these drugs increase ACE2 receptors coronavirus binds to. So someone had the bright idea of going through over 12,000 digital patients records to come up with the conclusion the drugs are safe to take and they do not cause worse symptoms. No animal studies, no clinical trials, and this was actually published.
“For the study, the researchers identified patients in the NYU Langone Health electronic health record with COVID-19 test results. For each identified patient with COVID-19 test results, the team discretely extracted medical history needed for the analysis, which compared treated and untreated patients.”
First you do a mouse study at least to review how coronavirus behaves in mice who are given the drugs, and compare it to mice not given the drugs. If science has been reduced to just going over records and coming to a conclusion, with no experimentation I have officially lost my mind.
Despite concerns expressed by some experts, common high blood pressure drugs did not increase the risk of contracting COVID-19 — or of developing severe disease — in a study of 12,594 patients.
Published online May 1 in the New England Journal of Medicine, the study was launched in response to a March 17 joint statement issued by the American Heart Association, the American College of Cardiology, and the Heart Failure Society of America. It urgently called for research to answer a question raised by past studies: do high blood pressure (antihypertensive) drugs worsen COVID-19 patient outcomes?
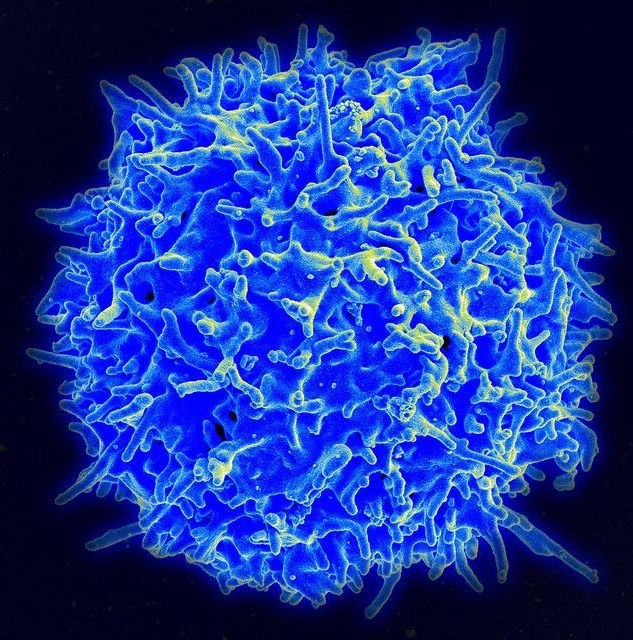
Led by researchers from NYU Grossman School of Medicine, the study found no links between treatment with four drug classes — angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta blockers, or calcium channel blockers — and increased likelihood of a positive test for COVID-19.