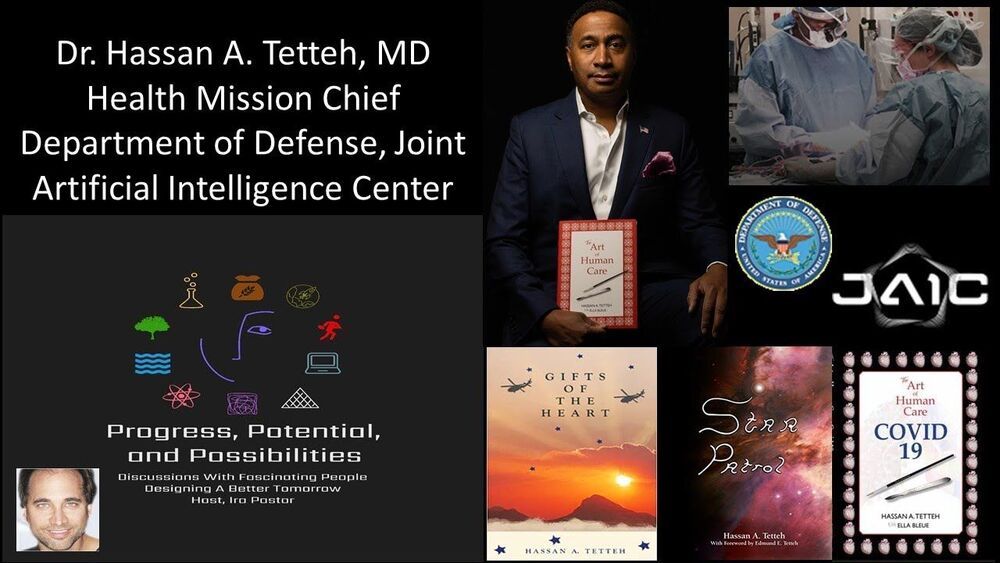
Dr. Hassan A. Tetteh, MD, is the Health Mission Chief, at the Department of Defense (DoD) Joint Artificial Intelligence Center, serving to advance the objectives of the DoD AI Strategy, and improve war fighter healthcare and readiness with artificial intelligence implementations.
Dr. Tetteh is also an Associate Professor of Surgery at the Uniformed Services University of the Health Sciences, adjunct faculty at Howard University College of Medicine, a Thoracic Staff Surgeon for MedStar Health and Walter Reed National Military Medical Center, and leads a Specialized Thoracic Adapted Recovery (STAR) Team, in Washington, DC, where his research in thoracic transplantation aims to expand heart and lung recovery and save lives.
In the past, Dr. Tetteh has served as Chief Medical Informatics Officer, United States Navy, and Division Lead for Futures and Innovation at Navy Medicine’s Headquarters, a Command Surgeon for the National Defense University, and as a Robert Wood Johnson Health Policy Fellow, assigned to the U.S. Congress, Congressional Budget Office, (CBO).
Dr. Tetteh served as Ship’s Surgeon and Director of Surgical Services for the USS Carl Vinson battle group in support of Operation Iraqi Freedom, deployed as a trauma surgeon to Afghanistan’s Helmand and Nimroz provinces in support of Operation Enduring Freedom, and has supported special joint forces missions to South America, the Middle East, the South Pacific, Australia, and Africa. He earned both the Surface Warfare Medical Department Officer and Fleet Marine Force Qualified Officer designations, and his military honors include two Meritorious Service Medals and the Joint Service Commendation Medal.
Dr. Tetteh is also an accomplished author, including the novel “Gifts of the Heart”, “Star Patrol” (co-authored with his son Edmund Tetteh), as well as “The Art of Human Care” and “The Art of Human Care for COVID-19″ (illustrated by his daughter Ella Bleue), and has published numerous articles on surgical innovation, health information technology, ethics, wounded warriors, and process improvement. He also serves on the board of directors for the Brooklyn, New York based Arthur Ashe Institute for Urban Health, Fayetteville, Arkansas based Champions for Kids, and Miriam’s Kitchen, a Washington, D.C. based nonprofit that works to end chronic homelessness.
Dr. Tetteh received his B.S. from State University of New York (SUNY), his M.D. from SUNY Downstate Medical Center, his M.P.A. from Harvard’s Kennedy School of Government, M.B.A. from Johns Hopkins University Carey Business School, and M.S. in National Security Strategy with a concentration in Artificial Intelligence from the National War College. He completed his thoracic surgery fellowship at the University of Minnesota and advanced cardiac surgery fellowship at Harvard Medical School’s Brigham and Women’s Hospital. Dr. Tetteh is a Certified Professional in Healthcare Information and Management, board certified in thoracic surgery, general surgery, clinical informatics, and healthcare management, and is a Fellow of the American College of Surgeons and Fellow of the American College of Healthcare Executives.