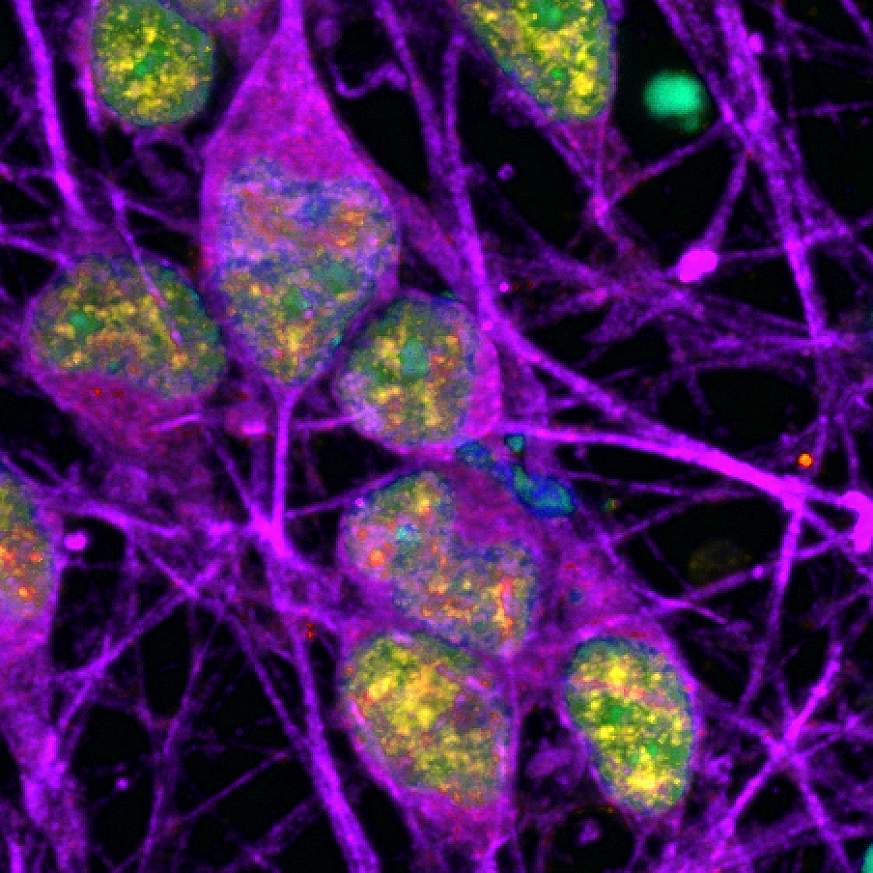
In the study, the researchers found that when AML cells were exposed to chemotherapy, a subset of the cells went into a state of hibernation, or senescence, while at the same time assuming a condition that looked very much like inflammation. They looked similar to cells that have undergone an injury and need to promote wound healing—shutting down the majority of their functions while recruiting immune cells to nurse them back to health.
Cancer cells can dodge chemotherapy by entering a state that bears similarity to certain kinds of senescence, a type of “active hibernation” that enables them to weather the stress induced by aggressive treatments aimed at destroying them, according to a new study by scientists at Weill Cornell Medicine. These findings have implications for developing new drug combinations that could block senescence and make chemotherapy more effective.
In a study published Jan. 26 in Cancer Discovery, a journal of the American Association for Cancer Research, the investigators reported that this biologic process could help explain why cancers so often recur after treatment. The research was done in both organoids and mouse models made from patients’ samples of acute myeloid leukemia (AML) tumors. The findings were also verified by looking at samples from AML patients that were collected throughout the course of treatment and relapse.
“Acute myeloid leukemia can be put into remission with chemotherapy, but it almost always comes back, and when it does it’s incurable,” said senior author Dr. Ari M. Melnick, the Gebroe Family Professor of Hematology and Medical Oncology and a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. “A longstanding question in the field has been, ‘Why can’t you get rid of all the cancer cells?’ A similar question can be posed for many other types of aggressive cancer in addition to AML.”