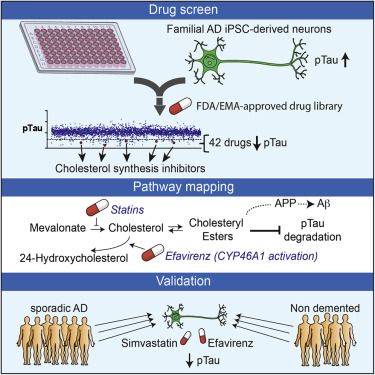
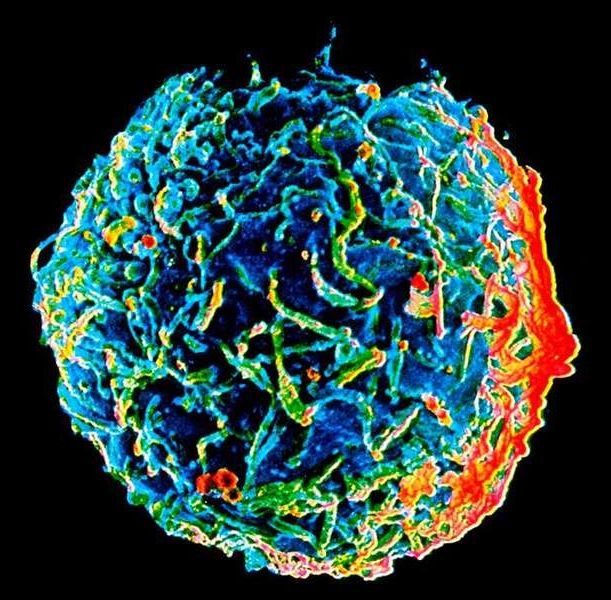
UC San Francisco scientists have used the CRISPR-Cas9 gene-editing system to create the first pluripotent stem cells that are functionally “invisible” to the immune system, a feat of biological engineering that, in laboratory studies, prevented rejection of stem cell transplants. Because these “universal” stem cells can be manufactured more efficiently than stem cells tailor-made for each patient—the individualized approach that dominated earlier efforts—they bring the promise of regenerative medicine a step closer to reality.
“Scientists often tout the therapeutic potential of pluripotent stem cells, which can mature into any adult tissue, but the immune system has been a major impediment to safe and effective stem cell therapies,” said Tobias Deuse, MD, the Julien I.E. Hoffman, MD, Endowed Chair in Cardiac Surgery at UCSF and lead author of the new study, published Feb. 18 in the journal Nature Biotechnology.
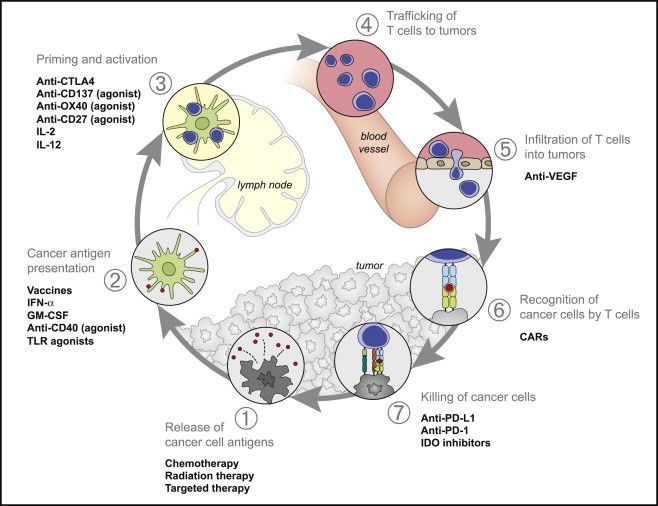
The immune system is unforgiving. It’s programmed to eradicate anything it perceives as alien, which protects the body against infectious agents and other invaders that could wreak havoc if given free rein. But this also means that transplanted organs, tissues or cells are seen as a potentially dangerous foreign incursion, which invariably provokes a vigorous immune response leading to transplant rejection. When this occurs, donor and recipient are said to be—in medical parlance—” histocompatibility mismatched.”
Read more