In 2017, Green Bay Packers quarterback Aaron Rodgers broke his right collarbone in a game against the Minnesota Vikings. Typically, it takes about 12 weeks for a collarbone to fully heal, but by mid-December fans and commentators were hoping the three-time MVP might recover early and save a losing season.
So did Xudong Wang, a professor of materials science and engineering at the University of Wisconsin-Madison and an expert in creating thin, movement-powered medical devices. “I started wondering if we could provide a new solution to bring athletes back to the field quicker than ever,” Wang says.
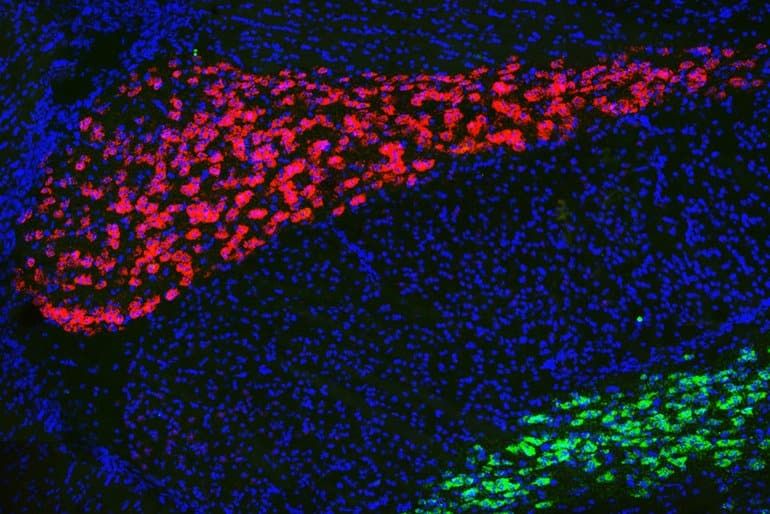
Researchers know that electricity can help speed up bone healing, but “zapping” fractures has never really caught on, since it requires surgically implanting and removing electrodes powered by an external source.
A major update of that same electrostimulation concept, Wang’s latest invention didn’t come in time to help the 2017 Packers–however, it may help many others by making electrostimulation a much more convenient option to speed up bone healing.
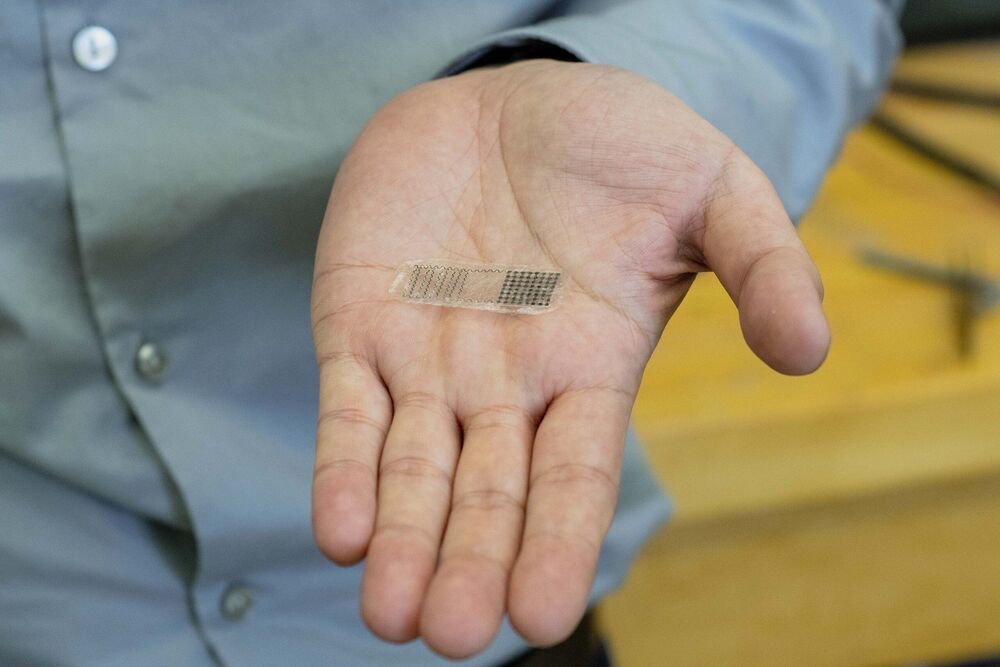
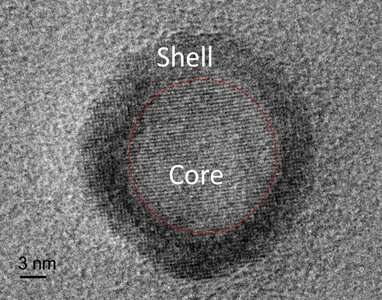
His thin, flexible device is self-powered, implantable and bioresorbable, so once the bone is knitted back together, the device’s components dissolve within the body.
Wang and his collaborators, including Weibo Cai, a UW-Madison professor of radiology and medical physics, described the new device today (July 5, 2021) in the journal Proceedings of the National Academy of Sciences.