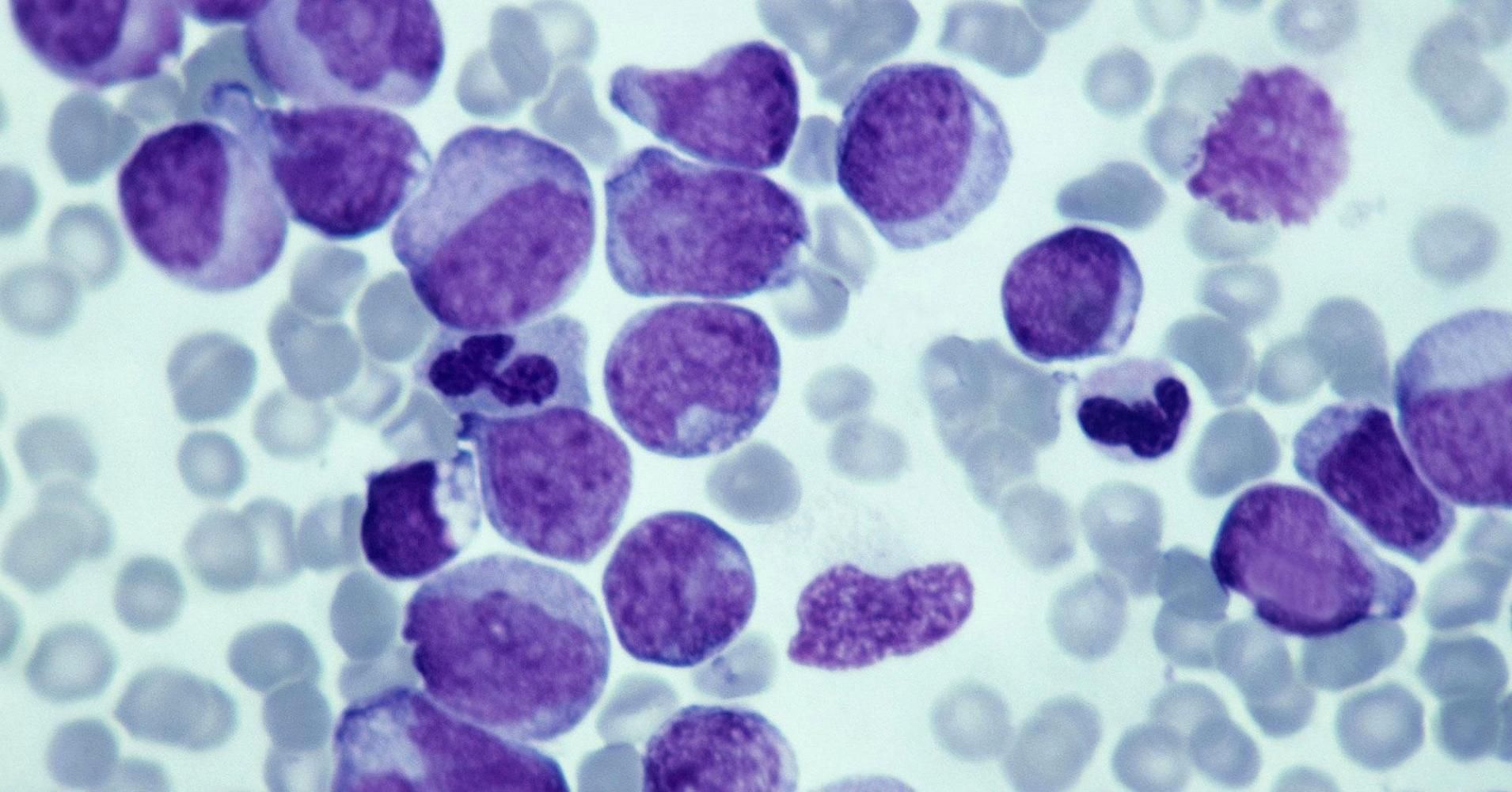
Cancer is devastating enough, and now this…
There is no sign of an imminent threat. But research suggests contagious human cancer could be possible. The New York Times reports.

Nathalie is agoraphobic and acrophobic, both anxiety disorders, the former involves fear of places or situations that may cause panic, the latter a pathological fear of heights.
To treat her doctors at the Van Gogh hospital in Charleroi, Belgium, are using virtual reality to help her control her fears.
Scientists are using virtual reality to treat bipolar disorder and phobias http://t.co/qR95oeCzLL pic.twitter.com/tWkJpUp5fl — Dave Asprey (@bulletproofexec) August 6, 2015

MindMaze has received $100 million to further medical research and launch a VR gaming system.
For a soldier who has endured an amputation, severe phantom limb pain can be debilitating.
Virtual reality company MindMaze has designed a medical virtual reality, augmented reality, and motion capture video game system that immerses the amputee in a virtual environment, where moving the existing arm will move the non-existing arm of the avatar. Neuroscientist and MindMaze founder and CEO Tej Tadi says this “mirroring” tricks the brain into believing the severed limb is actually there, and has proven benefits in phantom pain management.
Here is a concept; “could VR be used to rehabilitate criminals to experience through VR what their victims have experienced?” I do know in the recent 20 yrs a part of rehabilitation has included the criminal facing their victims so that the criminal develops a new level of empathy. However, could VR be a better solution? And, should it be?
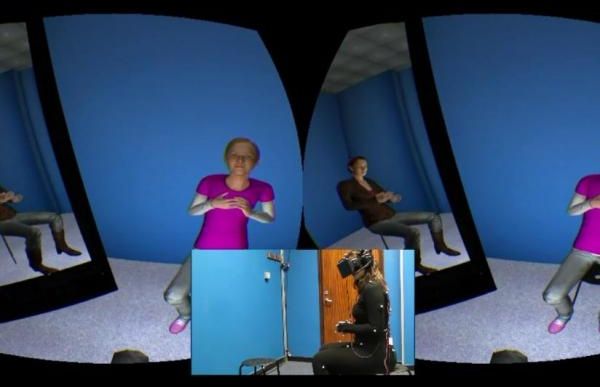
LONDON, Feb. 15 (UPI) — Depression patients who interacted with characters in a virtual reality environment were less critical and more compassionate toward themselves, researchers found in a small study in England.
Researchers at University College London found some of the self-directed negativity of people feel in depression can be mitigated through role-playing in virtual reality.
Dropping people into an immersive electronic world using a virtual reality headset gives them an opportunity to experience different scenarios — in this case, by embodying either somebody comforting a distressed child or by receiving the comfort as the distressed child.
People may soon use virtual reality to treat their depression and to be less critical and more compassionate towards themselves, a new study shows. A new virtual reality therapy has effectively reduced depressive symptoms of patients with some reporting significant drop in depression severity.
In the study, published in the British Journal of Psychiatry Open, patients claim virtual reality therapy changed their response to real-life situations in which they would previously have been self-critical.
The findings come from the analysis of the effect of the therapy to 15 depression patients, aged 23 to 61. Researchers, from University College London (UCL) and ICREA-University of Barcelona, asked the participants to wear a virtual reality headset to see from the perspective of a life-size “avatar” or virtual body.

Very interesting since many complex neural diseases also have ties to the brain stem such as Dystonia.
Feb. 22, 2016 — There is a new ground zero for Alzheimer’s Disease, according to a new discovery of a critical but vulnerable region in the brain that appears to be the first place affected by late onset Alzheimer’s disease. It also may be more important for maintaining cognitive function in later life than previously appreciated.
The locus coeruleus is a small, bluish part of the brainstem that releases norepinephrine, the neurotransmitter responsible for regulating heart rate, attention, memory, and cognition. Its cells, or neurons, send branch-like axons throughout much of the brain and help regulate blood vessel activity, says a new review of the scientific literature.
Its high interconnectedness may make it more susceptible to the effects of toxins and infections compared to other brain regions, said lead author Mara Mather.
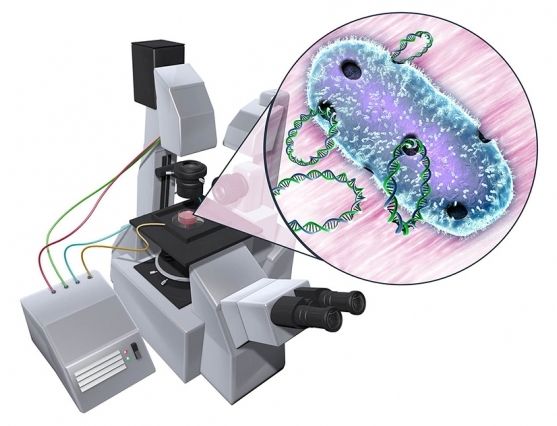
Breaking the bacteria barriers.
If that field is at just the right magnitude, it will open up pores within the cell membrane, through which DNA can flow. But it can take scientists months or even years to figure out the exact electric field conditions to reversibly unlock a membrane’s pores.
A new microfluidic device developed by MIT engineers may help scientists quickly home in on the electric field “sweet spot” — the range of electric potentials that will harmlessly and temporarily open up membrane pores to let DNA in. In principle, the simple device could be used on any microorganism or cell, significantly speeding up the first step in genetic engineering.
“We’re trying to reduce the amount of experimentation that’s needed,” said Cullen Buie, the Esther and Harold E. Edgerton Associate Professor of mechanical engineering at MIT. “Our big vision for this device and future iterations is to be able to take a process that usually takes months or years, and do it in a day or two.”

The job advertisement was highly specific: applicants had to be passionate about computer games and live in the UK. Oh, and they also had to be amputees who were interested in wearing a futuristic prosthetic limb.
James Young knew straight away he had a better shot than most. After losing an arm and a leg in a rail accident in 2012, the 25-year-old Londoner had taught himself to use a video-game controller with one hand and his teeth. “How many amputee gamers can there be?” he asked himself.
In the end, more than 60 people replied to the ad, which was looking for a games-mad amputee to become the recipient of a bespoke high-tech prosthetic arm inspired by Metal Gear Solid, one of the world’s best-selling computer games. Designed and built by a team of 10 experts led by London-based prosthetic sculptor Sophie de Oliveira Barata, the £60,000 carbon-fibre limb is part art project, part engineering marvel.
Great progress by Institute of the McGill University Health Centre has study astrocytes (the star shape brain cells) which play fundamental roles in nearly all aspects of brain function, could be adjusted by neurons in response to injury and disease.
A research team, led by the Research Institute of the McGill University Health Centre (RI-MUHC) in Montreal, has broken new ground in our understanding of the complex functioning of the brain. The research, which is published in the current issue of the journal Science, demonstrates that brain cells, known as astrocytes, which play fundamental roles in nearly all aspects of brain function, could be adjusted by neurons in response to injury and disease. The discovery, which shows that the brain has a far greater ability to adapt and respond to changes than previously believed, could have significant implications on epilepsy, movement disorders, and psychiatric and neurodegenerative disease.
Astrocytes are star-shaped cells in our brain that surround brain neurons, and neural circuits, protecting them from injury and enabling them to function properly – in essence, one of their main roles is to ‘baby-sit’ neurons. Our brain contains billions of cells, each of which need to communicate between each other in order to function properly. This communication is highly dependent on the behaviour of astrocytes. Until now, the mechanisms that create and maintain differences among astrocytes, and allow them to fulfill specialized roles, has remained poorly understood.
“It was believed that astrocytes acquired their properties during the development of the brain and then they were hardwired in their roles,” says senior study’s author Dr. Keith Murai, director of the Centre for Research in Neuroscience at the RI-MUHC, associate professor of the Department of Neurology and Neurosurgery at McGill University. “We have now discovered that astrocytes are actually incredibly flexible and potentially modifiable, which enables them to improve brain function or restore lost potential caused by disease.’’