Good question.
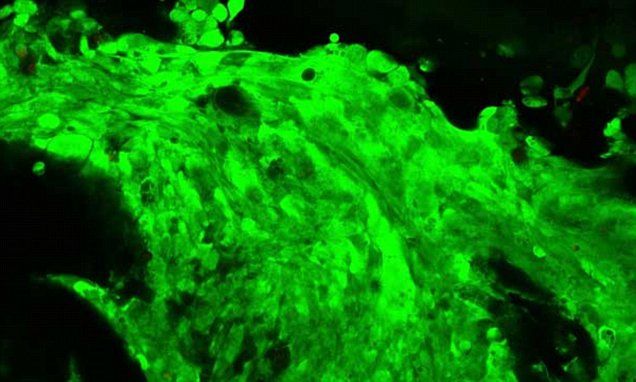
Tiny balls of cancerous cells are being printed off by researchers at Heriot Watt University in Edinburgh who hope it can provide new ways of testing drugs and studying brain cancers.



Interesting.
Futurists are accustomed to launching headfirst into some very complex subjects, but even the most high-minded and enthusiastic of prognosticators may take a pass when it comes to dealing with the future of sleep.
That’s no cop out.
It’s just that we humans — those in the developed world at least — maintain such a complicated relationship with sleep.
Awesome.
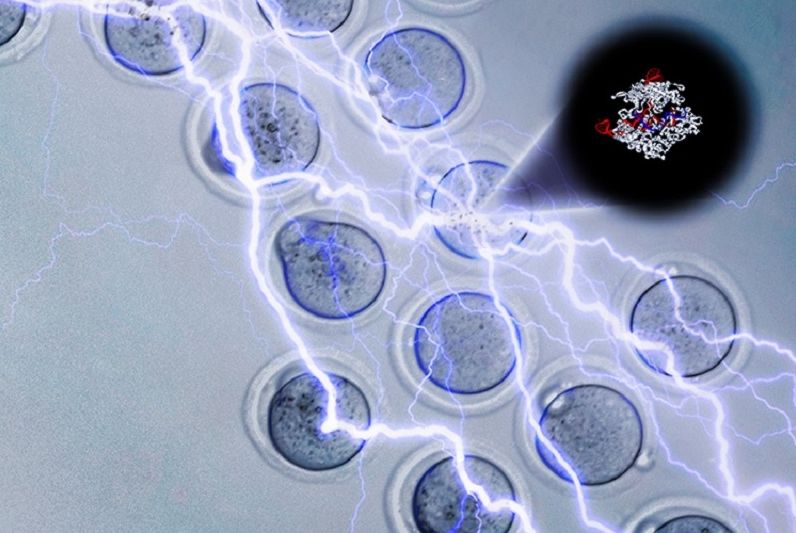
Researchers have developed a new gene editing tool that is more efficient and easier to use. CRISPR-EZ addresses the issue of target RNA accuracy and embryo viability in IVF transgenic mice.
( andrew modzelewski/lin he | university of california berkeley )
CRISPR gene editing has been the subject of many researchers around the world because of its great potential in the study human genetic disease. But more than that, scientists have high regard for this tool because it can help cure complex and debilitating diseases like dementia and cancer.
As more fine-tuning is done in the use of CRISPR gene editing, more diseases can be effectively cured. CRISPR-Cas9 has been used to accurately replace or change genes but it is mostly done in early embryos, and there is a need to increase its accuracy and ease of use. With this in mind, researchers from the University of California (UC) Berkeley have developed a new method called CRISPR-EZ (CRISPR ribonucleoprotein electroporation of zygotes) that would make gene editing easier.
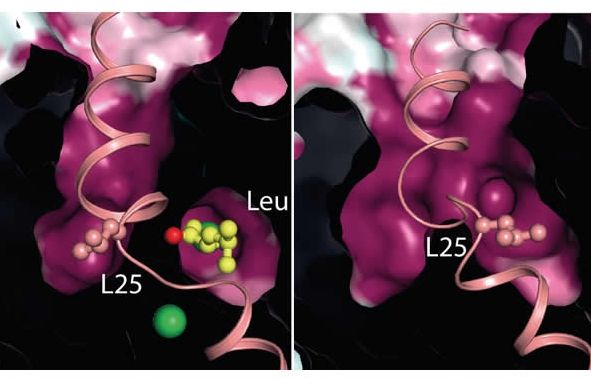
When nerve cells have to communicate with each other in our brains, it involves release of neurotransmitters acting as messengers at neural synapses. Here the released neurotransmitter is bound and registered by receptors at the surface of the receiving nerve cell. This will, in turn, trigger a signal which is sent on to other nerve cells. The circuits in the brain using the neurotransmitters noradrenaline, dopamine, GABA and serotonin are known to play an important role in mood, reward and mental well-being, and they also have a key role to in mental disorders such as addiction and depression.
After release of neurotransmitters between nerve cells, they must, however, be removed again to end the signal. This is done by a family of transport proteins which function as molecular vacuum cleaners in the cell membrane of the nerve cell where they pump the neurotransmitter back into the nerve cell for later reuse. This transport is of great importance to the signaling between the nerve cells, but happens relatively slowly. A collaborative project between researchers from Aarhus University has made it possible to explain what happens in the crucial rate-limiting step in the transport process for neurotransmitters such as serotonin, noradrenaline, GABA and dopamine which are all transported by related proteins with the same mechanism.


Interesting read on Chemo’s impact on the brain and brain functioning known as Chemo Brain.
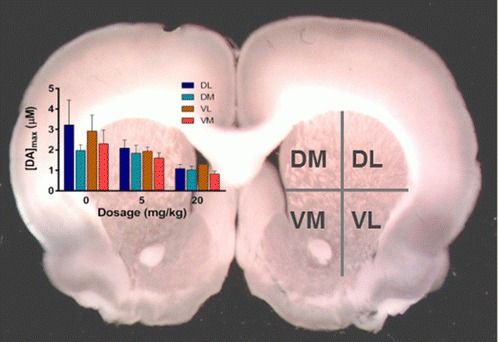
During and after chemotherapy, many cancer patients describe feeling a mental fog, a condition that has been dubbed “chemo brain.” Why this happens is unclear, but researchers have found a new clue to understanding this syndrome. A study in the journal ACS Chemical Neuroscience reports that chemotherapy in rats affects their chemical messengers dopamine and serotonin, which are associated with cognition.
Not surprised;
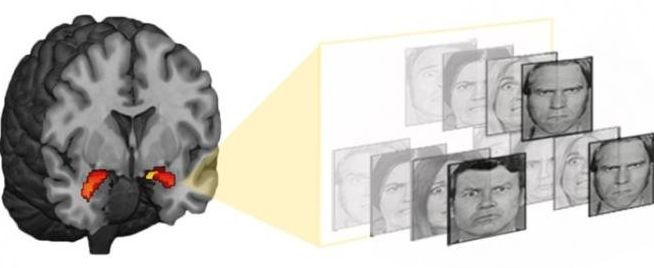
A long line of research links poverty and depression. Now, a study by Duke University scientists shows how biology might underlie the depression experienced by high-risk adolescents whose families are socio-economically disadvantaged.
The study, published May 24, 2016 in the journal Molecular Psychiatry, combined genetics, brain imaging and behavioral data gathered as adolescents were followed for more than three years as part of a larger study.
The results are part of a growing body of work that may lead to biological predictors that could guide individualized depression-prevention strategies.