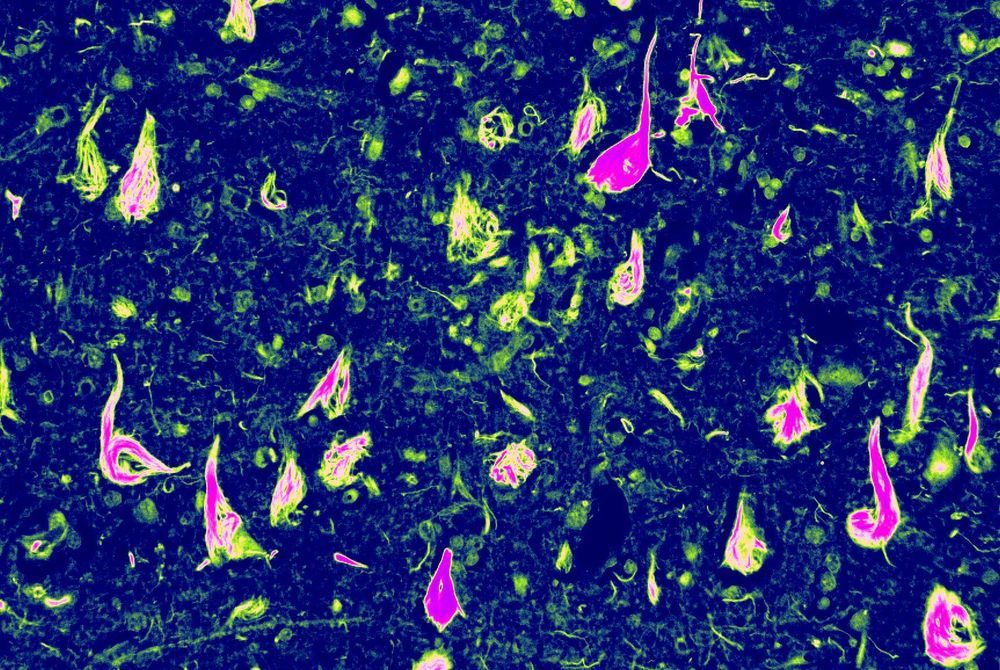
In the coming 2020s, the world of medical science will make some significant breakthroughs. Through brain implants, we will have the capability to restore lost memories.
~ The 2020s will provide us with the computer power to make the first complete human brain simulation. Exponential growth in computation and data will make it possible to form accurate models of every part of the human brain and its 100 billion neurons.
~ The prototype of the human heart was 3D printed in 2019. By the mid- 2020s, customized 3D- printing of major human body organs will become possible. In the coming decades, more and more of the 78 organs in the human body will become printable.
…As we enter into the next few decades, we will have the technologies that grant us the possibility of immortality, albeit one that is highly subjective.
With our ability to 3D print new body organs, our ability to use nanotechnology in fighting death at cellular levels, our ability to use CRISPR or other gene-editing technology to rewrite our definition of humans and even our ability to capture and extend our consciousness beyond the confines of the biological weakness of our human bodies — immortality may be within reach of our fingers as depicted in the painting of Michelangelo.
The race to human 2.0 will be run broadly in two spectrums — the evolution of our body and the evolution of our minds.
Excerpt from my book — 2020s & The Future Beyond.
#Future #Humanity #Transhumanism