While our circadian body clock dictates our preferred rhythm of sleep or wakefulness, a relatively new concept—the epigenetic clock—could inform us about how swiftly we age, and how prone we are to diseases of old age.
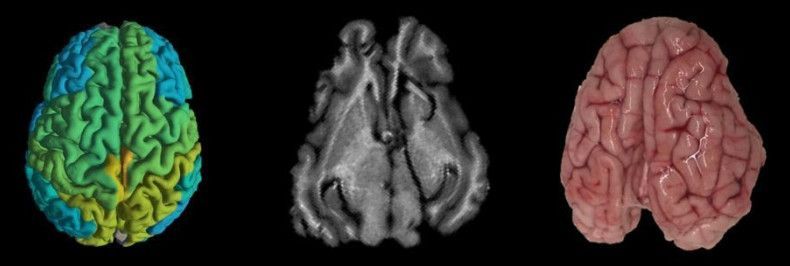
People age at different rates, with some individuals developing both characteristics and diseases related to aging earlier in life than others. Understanding more about this so-called ‘biological age’ could help us learn more about how we can prevent diseases associated with age, such as dementia. Epigenetic markers control the extent to which genes are switched on and off across the different cell-types and tissues that make up a human body. Unlike our genetic code, these epigenetic marks change over time, and these changes can be used to accurately predict biological age from a DNA sample.
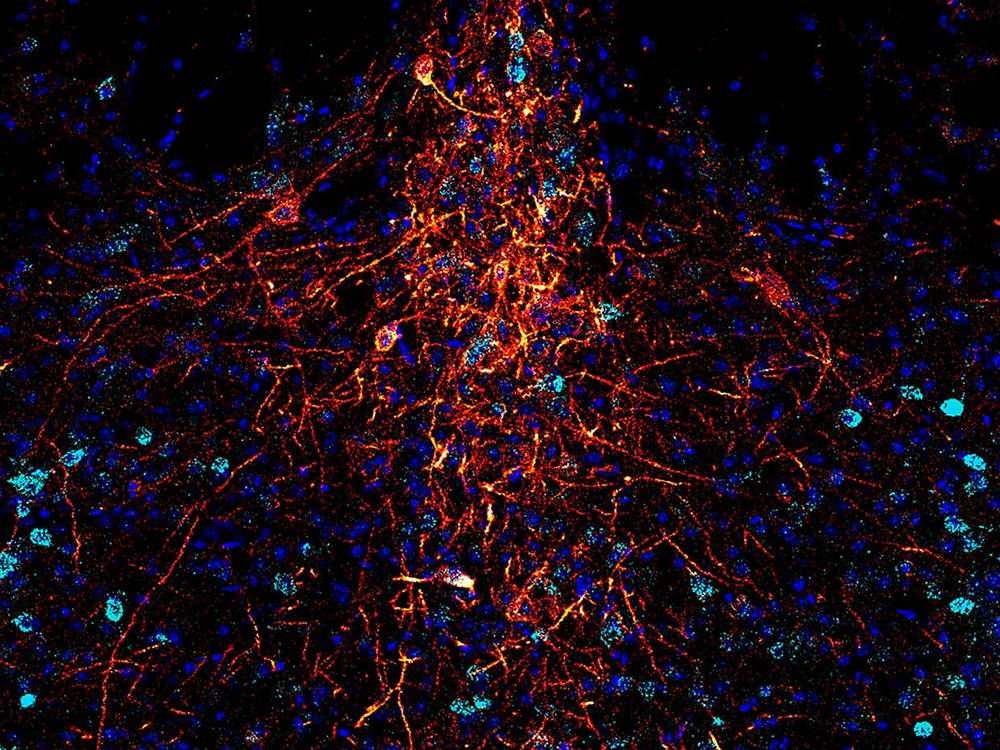
Now, scientists at the University of Exeter have developed a new epigenetic clock specifically for the human brain. As a result of using human brain tissue samples, the new clock is far more accurate than previous versions, that were based on blood samples or other tissues. The researchers hope that their new clock, published in Brain and funded by Alzheimer’s Society, will provide insight into how accelerated aging in the brain might be associated with brain diseases such as Alzheimer’s disease and other forms of dementia.



 Dr. David Sinefeld (Credit: Jerusalem College of Technology)
Dr. David Sinefeld (Credit: Jerusalem College of Technology)