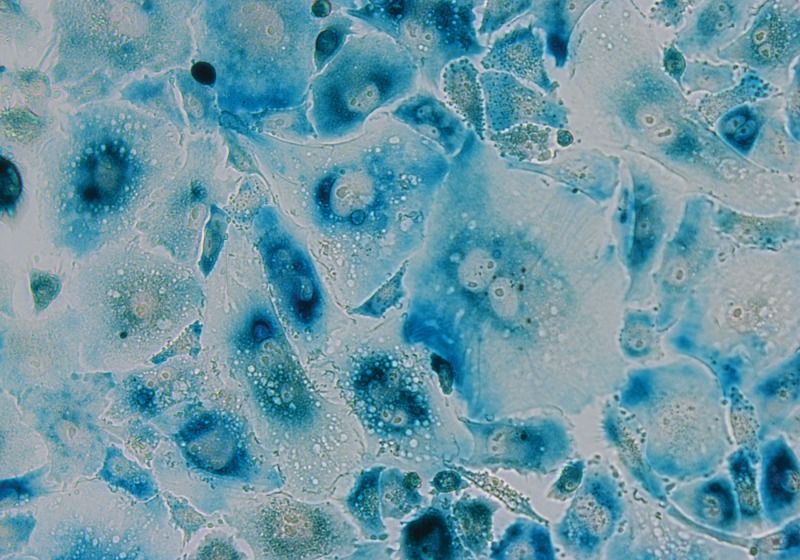
Researchers report an advance in the development of a blood test that could help detect pathological Alzheimer’s disease in people who are showing signs of dementia. This approach could be less invasive and less costly than current brain imaging and spinal fluid tests. The blood test detects the abnormal accumulation of a form of tau protein known as phosphorylated-tau-181 (ptau181), which is a biomarker that suggests brain changes from Alzheimer’s. The study, funded by the National Institutes of Health, was published on March 2 in Nature Medicine.
Over the past 15 years, research advances in the development of biomarkers like tau protein have enabled investigators to more accurately diagnose Alzheimer’s disease, select research participants, and measure response to investigational therapies. Tau and other biomarkers can be detected with PET scans of the brain and lab tests of spinal fluid. However, PET imaging is expensive and involves radioactive agents, and spinal fluid tests require spinal taps, which are invasive, complex and time-consuming. Simpler biomarker tests are still needed.
“The considerable time and resources required for screening research participants with PET scans and spinal taps slow the pace of enrollment for Alzheimer’s disease treatment studies,” said Richard J. Hodes, M.D., director of NIH’s National Institute on Aging (NIA), which funded much of the study. “The development of a blood test would enable us to rapidly screen a much larger and more diverse group of volunteers who wish to enroll in studies.”