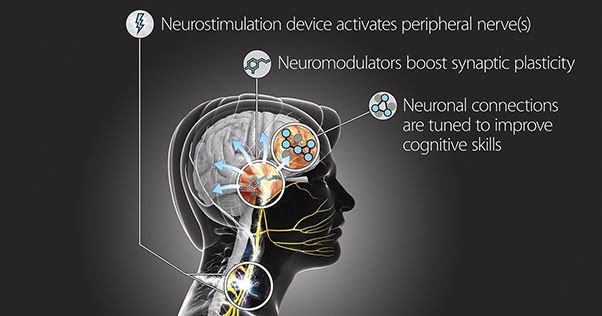
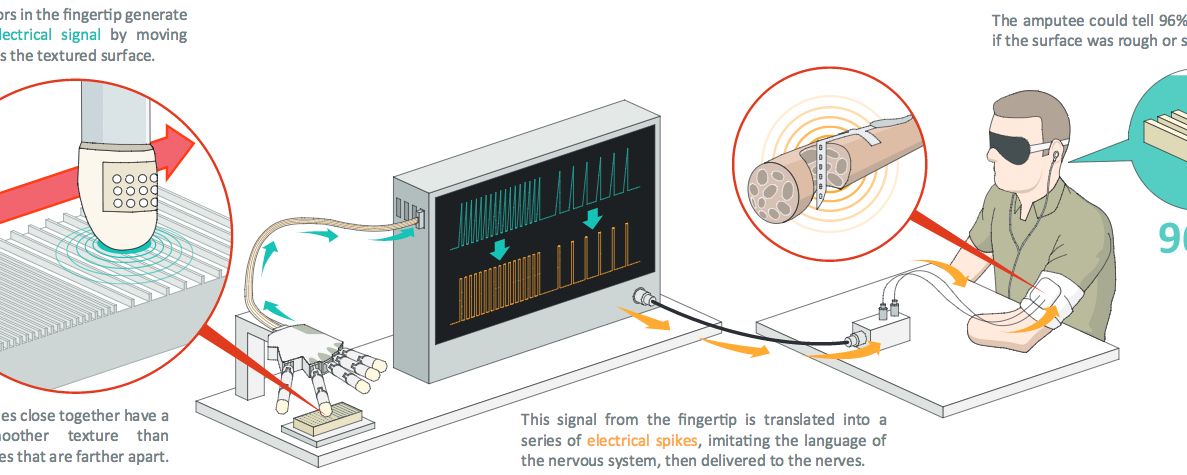
The body’s branching network of peripheral nerves connects neurons in the brain and spinal cord to organs, skin, and muscles, regulating a host of biological functions from digestion to sensation to locomotion. But the peripheral nervous system can do even more than that, which is why DARPA already has research programs underway to harness it for a number of functions—as a substitute for drugs to treat diseases and accelerate healing, for example, as well as to control advanced prosthetic limbs and restore tactile sensation to their users.
Now, pushing those limits further, DARPA aims to enlist the body’s peripheral nerves to achieve something that has long been considered the brain’s domain alone: facilitating learning. The effort will turn on its head the usual notion that the brain tells the peripheral nervous system what to do.
The new program, Targeted Neuroplasticity Training (TNT), seeks to advance the pace and effectiveness of a specific kind of learning—cognitive skills training—through the precise activation of peripheral nerves that can in turn promote and strengthen neuronal connections in the brain. TNT will pursue development of a platform technology to enhance learning of a wide range of cognitive skills, with a goal of reducing the cost and duration of the Defense Department’s extensive training regimen, while improving outcomes. If successful, TNT could accelerate learning and reduce the time needed to train foreign language specialists, intelligence analysts, cryptographers, and others.