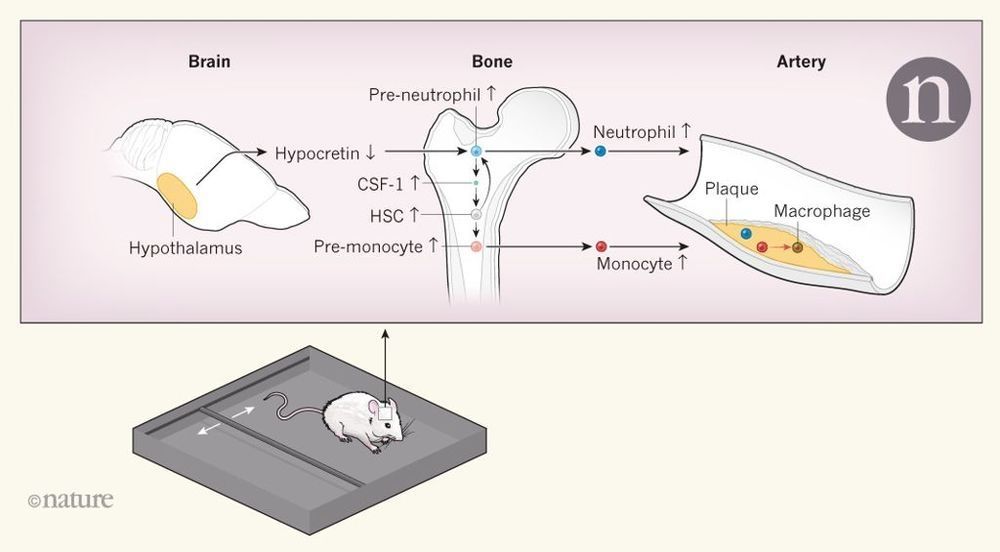
Most people have at some point echoed Macbeth’s complaint about the loss of “sleep that knits up the ravelled sleeve of care”. Sleep disorders, such as obstructive sleep apnoea (when breathing temporarily stops, causing both sleep disruption and lack of oxygen in blood) and sleep deprivation, have been associated with an increased risk of atherosclerosis and its harmful cardiovascular effects,. Atherosclerosis is characterized by the formation of ‘plaques’ in arteries, as white blood cells enter the artery wall, take up cholesterol and other substances from the blood and trigger an inflammatory response. However, the mechanisms linking sleep disruption and atherosclerosis have been largely unknown. Writing in Nature, McAlpine et al. show that persistent sleep disruption causes the brain to signal the bone marrow to increase the production of white blood cells.
McAlpine et al. studied mice that were prone to developing atherosclerosis. The authors induced sleep fragmentation by moving a bar intermittently across the bottom of the animals’ cages during their sleep period (Fig. 1), and compared these animals with animals that slept normally. They found that mice with sleep fragmentation had more-severe atherosclerosis, which was paralleled by increases in the production of white blood cells in the bone marrow and in the numbers of monocytes and neutrophils — two types of white blood cell — in the blood. These effects were absent if the bar was moved when the mice were fully awake. Stress activates the sympathetic nervous system (which is associated with the ‘fight-or-flight’ response), and such activation increases the production of white blood cells and atherosclerosis in other experimental settings. However, the authors did not find evidence for a role of sympathetic activation in their setting.